Understanding Diabetes and What Can Be Done
Diabetes is a serious disease that affects more than 170 million individuals globally and is the sixth most common cause of death in the United States. It occurs when the body has trouble transporting glucose, a form of sugar, out of the bloodstream and into the cells. Normally, when a healthy person eats a meal that contains glucose, the body’s blood-sugar level rises. In response, beta cells of the pancreas secrete a hormone called insulin, which lowers the high blood-glucose levels, into the bloodstream. Insulin does this by binding to surface proteins on the cells of the body, allowing glucose to enter the cell. Once glucose enters the cell, the cell breaks it down for the energy it needs to function properly.
Those with diabetes, however, fail to have enough insulin to maintain healthy levels of glucose in the bloodstream or in the cells. There are two known forms of this disease depending on how the body interacts with insulin: type 1 and type 2 diabetes. In type 1 diabetes, an autoimmune disease, the body’s own immune system targets the pancreatic beta cells. As a result, individuals with type 1 diabetes produce little to no insulin, so cells are not provided any glucose. The body’s immune system defends against foreign invaders. In this case, the immune system considers the beta cells as foreign invaders and attacks them. Individuals with type 2 diabetes, however, have insulin, but the cells cannot properly utilize normal insulin levels. Therefore, the cells ignore insulin’s signal to absorb and metabolize glucose. The body initially compensates by producing more insulin, but over time, the pancreas becomes overworked and reduces the amount of insulin it produces. Ultimately, both result in hyperglycemia, or severely high blood-sugar levels, which can have severe consequences on major organs of the body. In the worst cases, it can lead to conditions resulting in blindness, amputation, and, even, kidney failure.
Those with diabetes, however, fail to have enough insulin to maintain healthy levels of glucose in the bloodstream or in the cells. There are two known forms of this disease depending on how the body interacts with insulin: type 1 and type 2 diabetes. In type 1 diabetes, an autoimmune disease, the body’s own immune system targets the pancreatic beta cells. As a result, individuals with type 1 diabetes produce little to no insulin, so cells are not provided any glucose. The body’s immune system defends against foreign invaders. In this case, the immune system considers the beta cells as foreign invaders and attacks them. Individuals with type 2 diabetes, however, have insulin, but the cells cannot properly utilize normal insulin levels. Therefore, the cells ignore insulin’s signal to absorb and metabolize glucose. The body initially compensates by producing more insulin, but over time, the pancreas becomes overworked and reduces the amount of insulin it produces. Ultimately, both result in hyperglycemia, or severely high blood-sugar levels, which can have severe consequences on major organs of the body. In the worst cases, it can lead to conditions resulting in blindness, amputation, and, even, kidney failure.
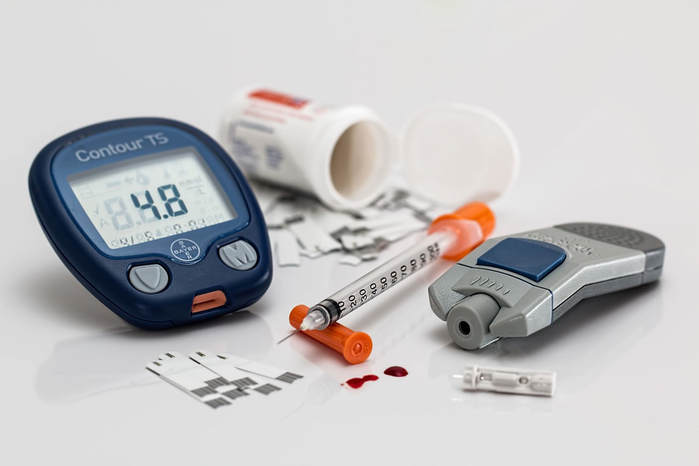
Image Source: stevepb
However, there are many ways for individuals to manage their conditions and regulate their blood-glucose levels. Since both types of diabetes involve the lack of insulin production, research has been devoted to finding ways of manually inserting insulin into patients’ bodies. For instance, since insulin is consumed when digested, one method of providing insulin is by injecting it under the skin where it can reach the bloodstream and eventually the cells. Another method involves a less painful procedure in which patients inhale a form of insulin into their bodies. It is also important to monitor blood-glucose levels regularly with a hemoglobin A1c test to assess whether a specific treatment is working and whether patients are in a healthy range. Type 1 diabetes patients may take immunosuppressants, which are medications that weaken the body’s immune system from attacking other cells in the body; as a result, the immune system would no longer attack the pancreas’ supply of insulin-producing beta cells.
In more extreme cases, diabetic patients may require surgery. For type 2 diabetes, patients may receive gastric reduction surgery, which reduces the capacity of the stomach. However, with this procedure, there may be complications that can include vomiting and leaks in the gastrointestinal system. For type 1 diabetes individuals, pancreatic transplants are an option to replace all the insulin producing cells. With any transplant, the immune system may consider the new organ as a foreign invader, so patients would need to take immunosuppressants.
In the early 20th century, having diabetes was virtually a death sentence as not much research had been devoted to the disease, and patients lacked the resources to manage their conditions. However, having the disease in the present is not as severe due to many clinical breakthroughs; deaths due to diabetes have decreased significantly in recent years due to the many methods of treatment. Patients with either type of diabetes can better manage their conditions and live relatively normal lives.
In more extreme cases, diabetic patients may require surgery. For type 2 diabetes, patients may receive gastric reduction surgery, which reduces the capacity of the stomach. However, with this procedure, there may be complications that can include vomiting and leaks in the gastrointestinal system. For type 1 diabetes individuals, pancreatic transplants are an option to replace all the insulin producing cells. With any transplant, the immune system may consider the new organ as a foreign invader, so patients would need to take immunosuppressants.
In the early 20th century, having diabetes was virtually a death sentence as not much research had been devoted to the disease, and patients lacked the resources to manage their conditions. However, having the disease in the present is not as severe due to many clinical breakthroughs; deaths due to diabetes have decreased significantly in recent years due to the many methods of treatment. Patients with either type of diabetes can better manage their conditions and live relatively normal lives.
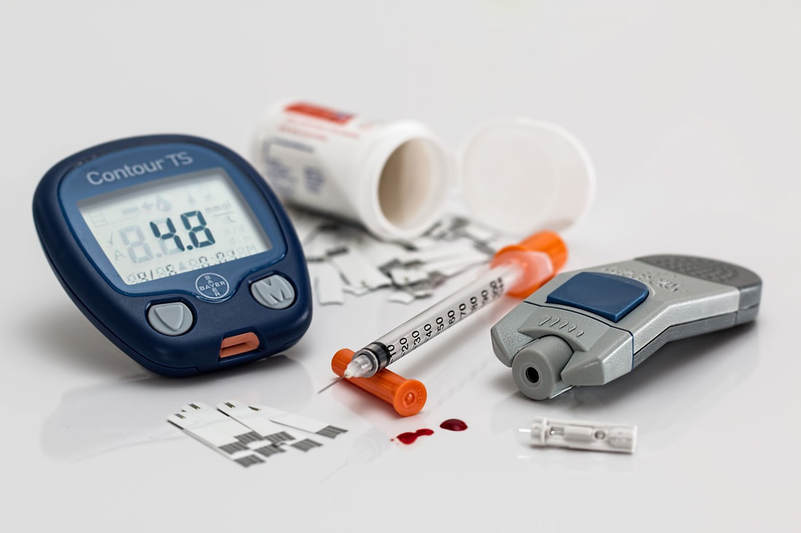
Featured Image Source: Tumisu
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|