Current Research and Therapies
Kate Santoso and Dhruv Khosla
Edited by Laila Khorasani
April 27 2021
Edited by Laila Khorasani
April 27 2021
Developing treatments for viral illnesses can be tricky, and COVID-19 is no exception. In order to survive, viruses depend on host cells for reproduction and metabolic processes. They use the cell’s machinery to produce more viral particles, which can multiply and take over an organism. Antiviral drugs must be able to target a particular part of a virus’s life cycle and destroy the virus without killing the human cells, in the case of SARS-CoV-2 (the virus that causes COVID-19). Viruses also reproduce quickly and undergo mutations that make developing antiviral drugs a challenge. COVID-19 variants have emerged in the United Kingdom, Brazil, and South Africa, and continue to worry scientists creating vaccines for distribution and current treatments.
Current treatments for those who are hospitalized with COVID-19 include the following drugs: dexamethasone, remdesivir, baricitinib in combination with remdesivir, and anticoagulation drugs (also known as blood thinners). Dexamethasone is a synthetic corticosteroid—a compound that imitates cortisol, a hormone naturally produced by the body—and is used to counter inflammation caused by the virus. Dexamethasone is administered to those who develop a hyperimmune response to COVID-19 and risk permanent damage to the lungs and other organs. It is used for those who need respiratory support. Another option for treating patients hospitalized with COVID-19 is the antiviral drug remdesivir, which was approved by the Food and Drug Administration (FDA) in October 2020, as the treatment has been proven to speed up recovery time. Remdesivir functions by stopping the virus from multiplying. Coronaviruses such as SARS-CoV-2 have genomes made of ribonucleic acid (RNA). Remdesivir interferes with an essential enzyme the virus needs to replicate its RNA and multiply.
Similarly, the use of baricitinib, an arthritis medication, in combination with remdesivir has also been approved for hospitalized patients who require respiratory support. Anticoagulation drugs are often administered to hospitalized COVID-19 patients to help prevent blood clots. These medications reduce the ability of blood to clot, which is important because a clot can disrupt the flow of blood to important organs.
Current treatments for those who are hospitalized with COVID-19 include the following drugs: dexamethasone, remdesivir, baricitinib in combination with remdesivir, and anticoagulation drugs (also known as blood thinners). Dexamethasone is a synthetic corticosteroid—a compound that imitates cortisol, a hormone naturally produced by the body—and is used to counter inflammation caused by the virus. Dexamethasone is administered to those who develop a hyperimmune response to COVID-19 and risk permanent damage to the lungs and other organs. It is used for those who need respiratory support. Another option for treating patients hospitalized with COVID-19 is the antiviral drug remdesivir, which was approved by the Food and Drug Administration (FDA) in October 2020, as the treatment has been proven to speed up recovery time. Remdesivir functions by stopping the virus from multiplying. Coronaviruses such as SARS-CoV-2 have genomes made of ribonucleic acid (RNA). Remdesivir interferes with an essential enzyme the virus needs to replicate its RNA and multiply.
Similarly, the use of baricitinib, an arthritis medication, in combination with remdesivir has also been approved for hospitalized patients who require respiratory support. Anticoagulation drugs are often administered to hospitalized COVID-19 patients to help prevent blood clots. These medications reduce the ability of blood to clot, which is important because a clot can disrupt the flow of blood to important organs.
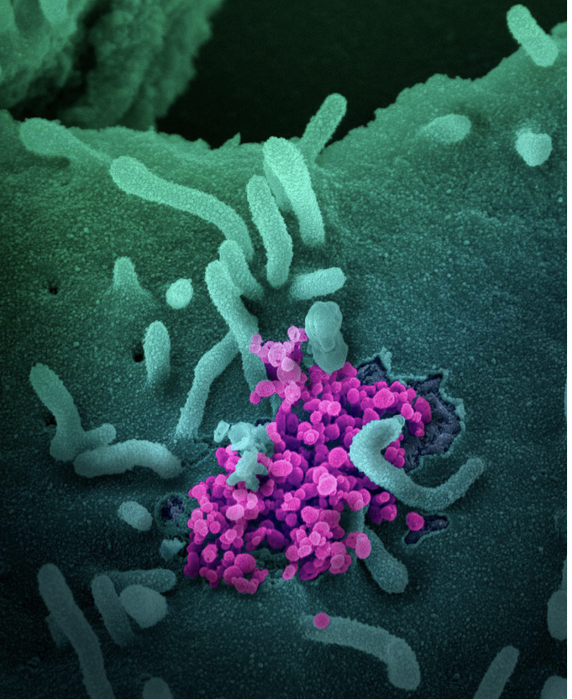
Image Source: NIH
When people recover from COVID-19, a part of their blood, called plasma, contains antibodies that the immune system produced to overcome the infection. Antibodies are proteins that fight off infections like viruses and protect the body should one become reinfected. The blood of people who recover from infectious diseases, including COVID-19, contains convalescent plasma and has been used for over 100 years to combat these diseases. In August 2020, the FDA issued emergency authorization to use convalescent plasma as a treatment for hospitalized COVID-19 patients. A clinical trial was done on patients 65 years of age and older to test whether convalescent plasma had an effect on outcomes. The researchers discovered that patients who received convalescent plasma within three days of developing symptoms were 48% less likely to develop severe COVID-19 illness compared to patients who received just the placebo. This treatment has benefits for those with COVID-19, particularly those at high risk of developing severe COVID-19.
Monoclonal antibody treatments are used for children older than 12 years of age and adults who have mild to moderate symptoms of COVID-19. They should be used for those who are at a high risk of more severe COVID-19 or being hospitalized. This treatment involves injecting man-made antibodies into the bloodstream to attack the coronavirus’s spike protein, making it difficult for the virus to infect cells. Three monoclonal antibody treatments have been authorized for emergency use by the FDA. However, no benefit for COVID-19 patients who are hospitalized or receiving oxygen therapy was seen in the clinical trials that tested them. Therefore, this form of treatment has not been authorized for treating this group.
Even with the development, production, and distribution of COVID-19 vaccines today, research for current therapies is still urgent as people continue to contract the virus and fall seriously ill. While 57.9 million people have been fully vaccinated in the United States since vaccine distribution began on December 14th, current treatments are essential to saving lives.
Monoclonal antibody treatments are used for children older than 12 years of age and adults who have mild to moderate symptoms of COVID-19. They should be used for those who are at a high risk of more severe COVID-19 or being hospitalized. This treatment involves injecting man-made antibodies into the bloodstream to attack the coronavirus’s spike protein, making it difficult for the virus to infect cells. Three monoclonal antibody treatments have been authorized for emergency use by the FDA. However, no benefit for COVID-19 patients who are hospitalized or receiving oxygen therapy was seen in the clinical trials that tested them. Therefore, this form of treatment has not been authorized for treating this group.
Even with the development, production, and distribution of COVID-19 vaccines today, research for current therapies is still urgent as people continue to contract the virus and fall seriously ill. While 57.9 million people have been fully vaccinated in the United States since vaccine distribution began on December 14th, current treatments are essential to saving lives.
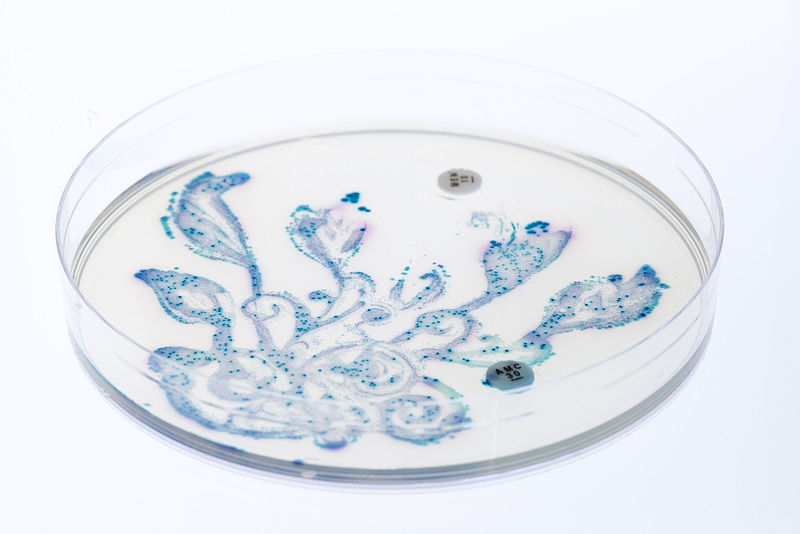
Featured Image Source: Pixabay
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|