The Emergence of "Superbugs": Are We Doomed Forever?
Ever since the first antibiotic was discovered in 1928, hundreds of millions of lives have been saved from deadly bacterial infections. Yet, the drug type’s newfound ubiquity now leads to an increasing amount of inappropriate uses. Whether it be a sore throat or common cold, people needlessly take antibiotics in the hopes that it will rid them of discomfort. Unfortunately, this leads to the development of multidrug resistant (MDR) bacteria, largely unfightable microbial strains that are predicted to kill over 10 million people by 2050.
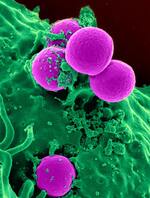
In 2013, the Centers for Disease Control and Prevention (CDC) labeled carbapenem-resistant Enterobacteriaceae as one of three MDR bacterial families that are the most threatening. This is quite serious since carbapenem is regularly prescribed as a treatment for severe bacterial infections. One of the most prevalent “superbugs” in this family is Klebsiella pneumoniae, a gram negative bacterium that is resident to the intestines but can cause severe infections if it colonizes other body tissues. In order to understand why it is resistant to carbapenem, it is first important to understand the meaning of the term “gram negative.”
In general, gram negative bacteria have developed a special kind of cell wall made up of three distinct segments: an inner layer, an outer layer, and a thin middle peptidoglycan layer. This middle element is essentially a large molecular cage-like network that protects the cell against both collapse and rupture. This layer is also rich in molecules like lipoprotein, which anchor the outer layer to the cell. Due to the large and diverse amount of these layers and linkages, antibiotics have a hard time diffusing into the bacteria. This highly developed drug resistance is part of what makes MDR bacteria so deadly.
In 2013, the Centers for Disease Control and Prevention (CDC) labeled carbapenem-resistant Enterobacteriaceae as one of three MDR bacterial families that are the most threatening. This is quite serious since carbapenem is regularly prescribed as a treatment for severe bacterial infections. One of the most prevalent “superbugs” in this family is Klebsiella pneumoniae, a gram negative bacterium that is resident to the intestines but can cause severe infections if it colonizes other body tissues. In order to understand why it is resistant to carbapenem, it is first important to understand the meaning of the term “gram negative.”
In general, gram negative bacteria have developed a special kind of cell wall made up of three distinct segments: an inner layer, an outer layer, and a thin middle peptidoglycan layer. This middle element is essentially a large molecular cage-like network that protects the cell against both collapse and rupture. This layer is also rich in molecules like lipoprotein, which anchor the outer layer to the cell. Due to the large and diverse amount of these layers and linkages, antibiotics have a hard time diffusing into the bacteria. This highly developed drug resistance is part of what makes MDR bacteria so deadly.
Image Source: Pixabay
Presented with these problems, researchers at Rice University recently developed a “molecular drill” that burrows through these layers once activated by light, allowing antibiotics to more easily pass through. Because these drills are powered by mechanical action and not chemical effects, bacteria cannot produce biological resistance against them. Due to this, numerous tests indicated that the researchers were able to kill 94% of K. pneumonia in the lab by supplementing carbapenem with a careful balance of these molecular drills.
Although these molecular nanomachines have the potential to save millions of lives, they are not without their limitations. Primarily, these drills require light energy to be activated. As such, infections on an outer tissue layer, such as the surface of the skin, could be easily fought by the actions of these drills. However, if the infection were bloodborne, it would be challenging to activate them with light. Furthermore, the requisite light source must correspond to a wavelength of 365 nm (ultraviolet light). This presents further problems, as this form of light energy may alter gene expression. With these limitations aside, however, molecular drills now represent a new avenue in the fight for eliminating MDR bacteria.
Although these molecular nanomachines have the potential to save millions of lives, they are not without their limitations. Primarily, these drills require light energy to be activated. As such, infections on an outer tissue layer, such as the surface of the skin, could be easily fought by the actions of these drills. However, if the infection were bloodborne, it would be challenging to activate them with light. Furthermore, the requisite light source must correspond to a wavelength of 365 nm (ultraviolet light). This presents further problems, as this form of light energy may alter gene expression. With these limitations aside, however, molecular drills now represent a new avenue in the fight for eliminating MDR bacteria.
Featured Image Source: Chokniti Khongchum
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|