Activating the Killer in Stem Cells to Improve Cancer Immunotherapy
“You have cancer” is one of the most frightening diagnoses one can hear today. Caused by uncontrolled cell growth leading to the formation of malignant tumors, cancers of various kinds are diagnosed in approximately 1.8 million people in the U.S alone every year, and millions more worldwide. Oncology researchers are working around the clock to develop better treatments, and one day perhaps even produce a cure.
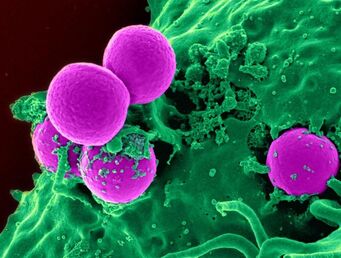
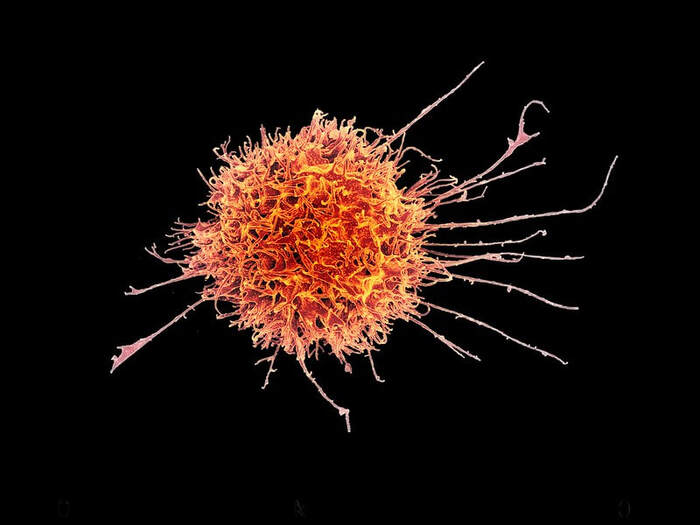
For now, one kind of treatment plan available involves cancer inhibition therapy, which works by manipulating the immune system response. Cancer inhibition therapy primarily targets T cells, a type of white blood cell that protects the body from harmful pathogens. This can be done with immune checkpoint inhibitors, drugs that act on checkpoint proteins, which are molecules on the surface of T cells that regulate the cell’s response to foreign substances. In a cancer patient, when checkpoint proteins on the T cell bind to a cancerous cell, a signal is sent back to the T cell that “turns off” or deactivates the T cell. This is eventually fatal for the patient, as now the T cell will no longer destroy the tumor as it would in healthy people. Cancer inhibition therapy through the use of immunotherapy drugs seeks to reverse this process by preventing T cells from binding to cancer cells, thus allowing unbound T cells to attack and destroy tumors as desired. This process can be further enhanced by using natural killer (NK) cells in addition to the drugs, which bolster immune response by directly attacking identified cancerous cells.
For now, one kind of treatment plan available involves cancer inhibition therapy, which works by manipulating the immune system response. Cancer inhibition therapy primarily targets T cells, a type of white blood cell that protects the body from harmful pathogens. This can be done with immune checkpoint inhibitors, drugs that act on checkpoint proteins, which are molecules on the surface of T cells that regulate the cell’s response to foreign substances. In a cancer patient, when checkpoint proteins on the T cell bind to a cancerous cell, a signal is sent back to the T cell that “turns off” or deactivates the T cell. This is eventually fatal for the patient, as now the T cell will no longer destroy the tumor as it would in healthy people. Cancer inhibition therapy through the use of immunotherapy drugs seeks to reverse this process by preventing T cells from binding to cancer cells, thus allowing unbound T cells to attack and destroy tumors as desired. This process can be further enhanced by using natural killer (NK) cells in addition to the drugs, which bolster immune response by directly attacking identified cancerous cells.
Cancer inhibition therapy, although relatively effective, is not without its limitations. For instance, some cancerous tumors have genetic mutations which have developed resistance to the immunotherapy drugs. Another problem is that NK cells, which can boost the treatment, are not a naturally abundant resource. Only one to two doses can be harvested from a single donor, and the cell extraction can be expensive. Therefore, researchers such as Frank Cichocki and his team from the University of Minnesota have been seeking ways to address these concerns and enhance immunotherapy treatment.
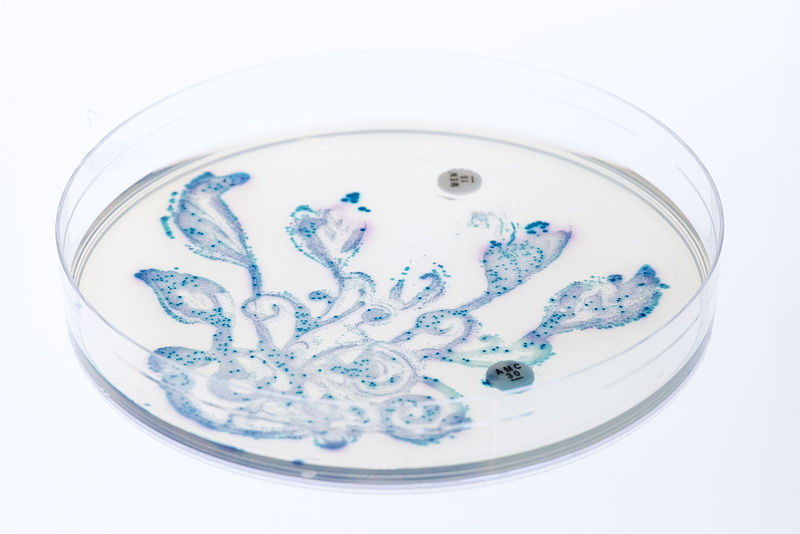
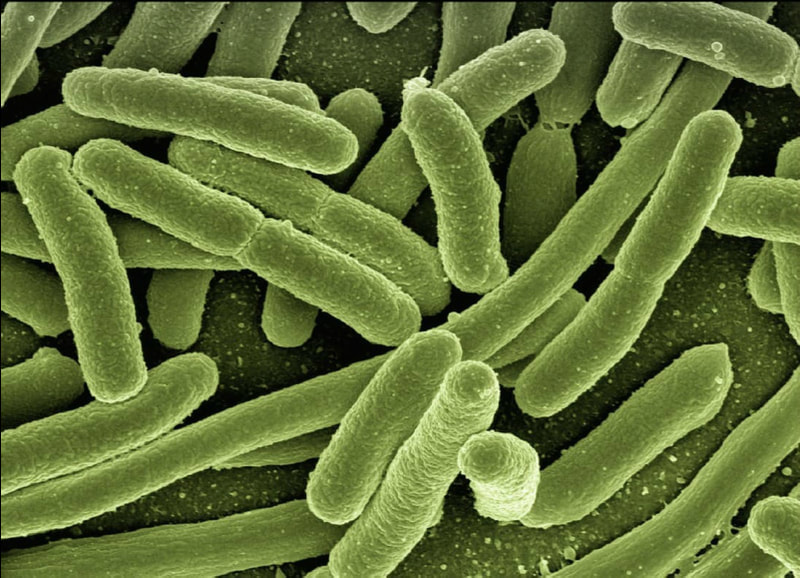
Described in a paper published in November 2020, Cichocki’s team developed a system which manipulates induced pluripotent stem cells (iPSCs) to turn them into more NK cells, thus creating induced pluripotent stem cell-derived natural killer (iNK) cells. After manufacturing iNK cells, they tested their efficacy against various types of cancer cells in three different stages by using bioluminescence imaging, cell cultures, and lab mice. After inserting ovarian cancer cells in mice, along with varying combinations of iNK cells, T cells, and anti-PD-1 antibodies, the researchers found that tumors were significantly reduced in mice who had the treatment compared to those who did not. They also found that cancerous mice with iNK cells had higher survival rates than those without them.
Cichocki and his team concluded that the iNK cells increased the production of cytokines (a type of protein that aids cell signaling), helped recruit and activate more T cells, and created a toxic environment for tumors. The combination of these effects amplified the effect of pre-existing immunotherapy treatments and directly attacked malignant cells, potentially improving the quality of cancer inhibition therapy.
The researchers have since developed a drug containing iNK cells, and their investigator new drug application has been approved by the US Food and Drug Administration. It is currently being used in clinical trials with advanced cancer patients. If the drug is as effective in humans as it was in mice, it could significantly reduce the impact of tumors on the body—one step closer to killing cancer once and for all.
Described in a paper published in November 2020, Cichocki’s team developed a system which manipulates induced pluripotent stem cells (iPSCs) to turn them into more NK cells, thus creating induced pluripotent stem cell-derived natural killer (iNK) cells. After manufacturing iNK cells, they tested their efficacy against various types of cancer cells in three different stages by using bioluminescence imaging, cell cultures, and lab mice. After inserting ovarian cancer cells in mice, along with varying combinations of iNK cells, T cells, and anti-PD-1 antibodies, the researchers found that tumors were significantly reduced in mice who had the treatment compared to those who did not. They also found that cancerous mice with iNK cells had higher survival rates than those without them.
Cichocki and his team concluded that the iNK cells increased the production of cytokines (a type of protein that aids cell signaling), helped recruit and activate more T cells, and created a toxic environment for tumors. The combination of these effects amplified the effect of pre-existing immunotherapy treatments and directly attacked malignant cells, potentially improving the quality of cancer inhibition therapy.
The researchers have since developed a drug containing iNK cells, and their investigator new drug application has been approved by the US Food and Drug Administration. It is currently being used in clinical trials with advanced cancer patients. If the drug is as effective in humans as it was in mice, it could significantly reduce the impact of tumors on the body—one step closer to killing cancer once and for all.
Featured Image Source: Pixabay
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|