How a Tiny Machine Creates Inequality in Healthcare
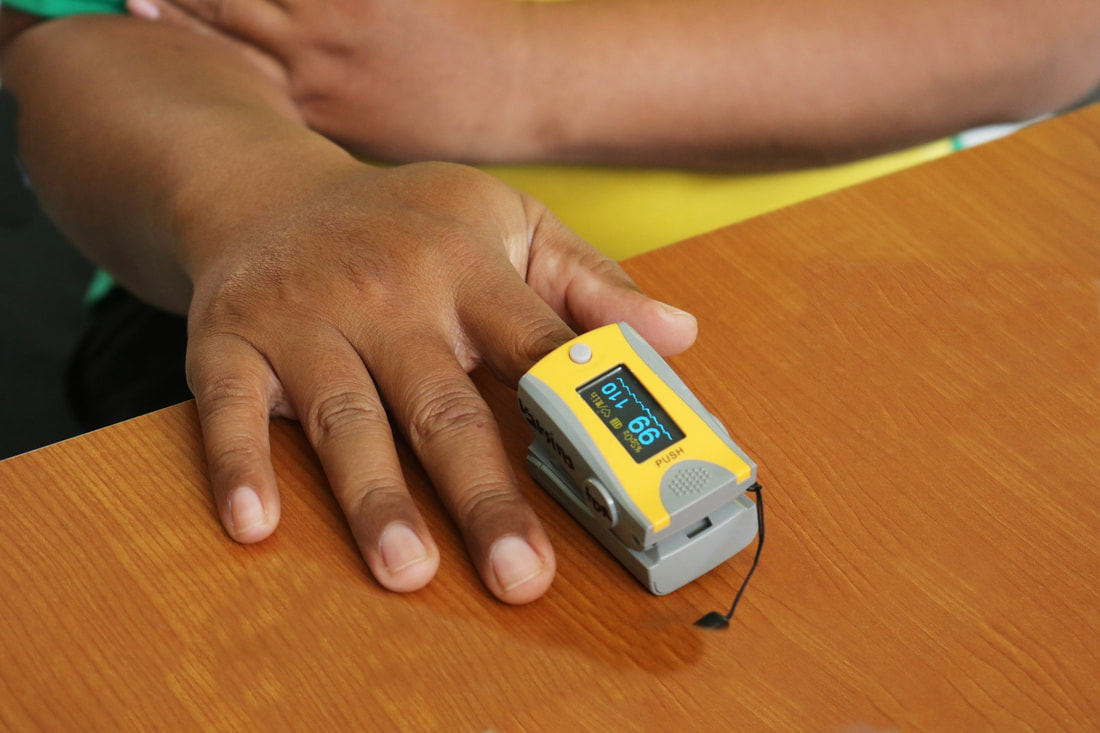
Hemoglobin proteins work as tiny delivery trucks in the bloodstream to make sure that oxygen is delivered from the respiratory system to the rest of the body. If hemoglobin proteins don’t carry enough oxygen in the blood, a state known as hypoxemia, the rest of the body may not work properly. To easily check blood oxygen levels at home without drawing blood, a device called a pulse oximeter was created.
Pulse oximeters use lasers to estimate oxygen saturation, the amount of oxygen carried by hemoglobin. Because they use light as a sensor, changes to surface color, such as adding nail polish or having a darker skin color, affect the way that they read the oxygen values. This happens because darker colors are more likely to block the laser from being able to read blood oxygen levels. Typically, this means that White patients are more likely to get an accurate reading of their oxygen saturation level through a pulse oximeter reading than BIPOC (Black, Indigenous, and people of color) patients would. Not only does this mean that BIPOC patients would be less likely to be diagnosed with hypoxemia, but it also means that they are less likely to get urgent treatment for other related diseases, such as COVID-19. This is one of the reasons why population treatment disparities exist across racial and ethnic groups.
Pulse oximeters use lasers to estimate oxygen saturation, the amount of oxygen carried by hemoglobin. Because they use light as a sensor, changes to surface color, such as adding nail polish or having a darker skin color, affect the way that they read the oxygen values. This happens because darker colors are more likely to block the laser from being able to read blood oxygen levels. Typically, this means that White patients are more likely to get an accurate reading of their oxygen saturation level through a pulse oximeter reading than BIPOC (Black, Indigenous, and people of color) patients would. Not only does this mean that BIPOC patients would be less likely to be diagnosed with hypoxemia, but it also means that they are less likely to get urgent treatment for other related diseases, such as COVID-19. This is one of the reasons why population treatment disparities exist across racial and ethnic groups.
Image Source: Vector8DIY
But how do pulse oximetry readings have an effect on the way certain people receive treatment in hospitals? When it comes to patients admitted into the Intensive Care Unit (ICU), Black patients typically have a lower oxygen saturation level than White, Hispanic, and Asian patients, who all have similar oxygen saturation levels. However, when pulse oximeters are used, on average Black patients reported having a higher pulse oximeter reading than White patients. Despite having similar oxygen saturation levels to White patients, Hispanic and Asian patients also received a higher estimate from the pulse oximeters, although not as high as black patients. Because of this, Black and Asian patients had a lower rate of receiving oxygen treatments than White patients, and Hispanic patients were becoming less likely to receive oxygen treatments over time when compared to White patients.
This disparity occurs due to the different ways of approximating oxygen saturation levels in the bloodstream. When you compare how likely a patient is to receive oxygen treatment to their oxygen saturation level, as reported by a pulse oximeter, there doesn’t seem to be any difference in how different races/ethnicities are treated and it appears that everyone is getting the amount of treatment that they deserve. However, when oxygen saturation level is measured by taking blood samples, which is a far more accurate way of measurement, the treatment disparities between different racial and ethnic groups are more obvious. Thus, Black, Asian, and Hispanic patients are less likely to receive oxygen treatments because of the lack of accuracy from pulse oximeters.
This issue is not only relevant in terms of health disparities between populations, but also in terms of other potential treatments in the future. There may be increased use of machines that automatically supply oxygen to patients based on their pulse oximeter reading, and if that reading is inaccurate, it could result in a worsening treatment disparity. In an ideal world, these readings would be corrected based on color readings and not race; however, it’s important to understand the racial background behind this issue. Once we recognize the reasons behind a problem, we can work towards making a more equitable world in healthcare.
This disparity occurs due to the different ways of approximating oxygen saturation levels in the bloodstream. When you compare how likely a patient is to receive oxygen treatment to their oxygen saturation level, as reported by a pulse oximeter, there doesn’t seem to be any difference in how different races/ethnicities are treated and it appears that everyone is getting the amount of treatment that they deserve. However, when oxygen saturation level is measured by taking blood samples, which is a far more accurate way of measurement, the treatment disparities between different racial and ethnic groups are more obvious. Thus, Black, Asian, and Hispanic patients are less likely to receive oxygen treatments because of the lack of accuracy from pulse oximeters.
This issue is not only relevant in terms of health disparities between populations, but also in terms of other potential treatments in the future. There may be increased use of machines that automatically supply oxygen to patients based on their pulse oximeter reading, and if that reading is inaccurate, it could result in a worsening treatment disparity. In an ideal world, these readings would be corrected based on color readings and not race; however, it’s important to understand the racial background behind this issue. Once we recognize the reasons behind a problem, we can work towards making a more equitable world in healthcare.
Featured Image Source: mufidpwt
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|