What You Eat May Change How Your Body Wants to Eat
It is widely understood that consuming a high-calorie diet rich in fat and sugar can lead to obesity. Indeed, besides excessive body fat, obesity may also involve elevated blood pressure and increased levels of sugar, fat, and cholesterol in the blood. Moreover, obesity increases the risk of a number of other chronic conditions, such as diabetes, depression, and fatty liver disease, as well as acute illnesses, including heart attack and stroke.
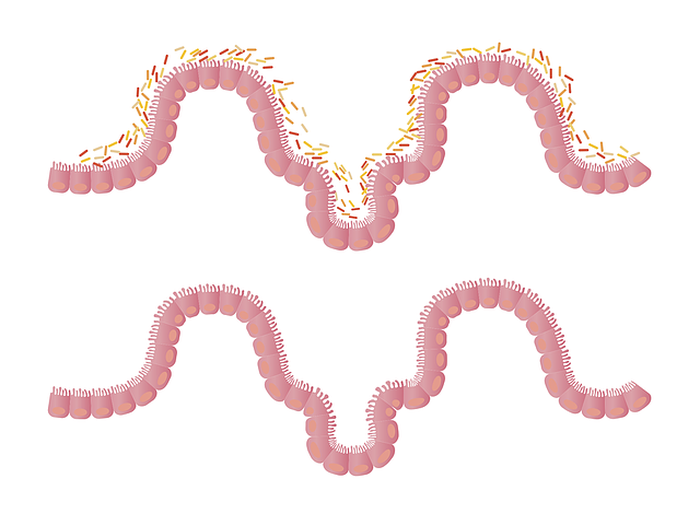
Although healthy eating is beneficial in preventing obesity, the physiological processes that regulate eating behaviors may be harder to control. One such process is signaling by molecules to neurons in the hypothalamus, the part of the brain that maintains the energy “budget” of the body. For example, the hormone leptin produced by fat cells signals to the hypothalamus, inhibiting the production of a molecule called neuropeptide Y (NPY) in the nervous system, reducing appetite. Another molecule called galanin and its receptor were previously found to stimulate consumption of fat. Yet another important component of energy intake is the gut microbiota, or bacteria in the digestive system, which have been found to affect feeding behavior.
Therefore, to understand the development of obesity as primarily caused by unhealthy eating, it is necessary to examine how these biological features change in response to high calorie intake. As such, in a study published in the Journal of Nutritional Biochemistry, researchers studied changes in signaling molecule levels and the gut microbiota in mice, as well as whether these factors may be correlated, when obesity was induced by a high-sugar and fat (HSB) diet.
Although healthy eating is beneficial in preventing obesity, the physiological processes that regulate eating behaviors may be harder to control. One such process is signaling by molecules to neurons in the hypothalamus, the part of the brain that maintains the energy “budget” of the body. For example, the hormone leptin produced by fat cells signals to the hypothalamus, inhibiting the production of a molecule called neuropeptide Y (NPY) in the nervous system, reducing appetite. Another molecule called galanin and its receptor were previously found to stimulate consumption of fat. Yet another important component of energy intake is the gut microbiota, or bacteria in the digestive system, which have been found to affect feeding behavior.
Therefore, to understand the development of obesity as primarily caused by unhealthy eating, it is necessary to examine how these biological features change in response to high calorie intake. As such, in a study published in the Journal of Nutritional Biochemistry, researchers studied changes in signaling molecule levels and the gut microbiota in mice, as well as whether these factors may be correlated, when obesity was induced by a high-sugar and fat (HSB) diet.
Image Source: Shutterbug75
The researchers did two rounds of comparisons, each round with 12 mice. The mice were first fed a standard diet, then divided into two groups, with one group now receiving the HSB diet, which contained less protein and much more fat. After 12 weeks, the researchers saw many of the aforementioned obesity-like traits in the HSB mice, such as weight gain, excessive liver fat, and high blood sugar and fat levels. The adiposity index, or body fat percentage, of these mice was also larger. Behavioral tests revealed that HSB mice not only showed more obsessive-compulsive-like behaviors but also experienced reduced anxiety, likely due to activation of the brain reward system by the HSB diet. Levels of signaling molecules also changed in these mice—higher amounts of leptin, NPY, galanin, and galanin receptors were produced due to a prolonged HSB diet. Interestingly, the abundances of many different species of gut bacteria were also different in HSB mice. Moreover, it was found that the relative abundances of gut microbiota species correlated with several of the other traits, including the adiposity index, obsessive-compulsive-like behavior, and amounts of neuropeptides.
Many of these results agree with existing findings under different settings and may improve studies in humans. This study supported the idea that the anxiety-reducing effect of a HSB diet can lead to reliance on this diet as a compulsive behavior. The increased levels of signaling molecules found suggest that under this diet, the body no longer properly responds to the signaling pathway that regulates appetite. Most importantly, the observed change in gut microbiota composition not only supports previous studies, but its correlation with other results also points to how it can directly affect feeding behavior and brain signaling, thereby contributing to obesity. Researchers hope to further confirm this by transferring gut microbiota from HSB mice to normal mice and observing the effects. As specific species of gut microbiota that play critical roles in the development of obesity are identified, scientists may be able to design treatments that target these species to slow or prevent disease progression.
Many of these results agree with existing findings under different settings and may improve studies in humans. This study supported the idea that the anxiety-reducing effect of a HSB diet can lead to reliance on this diet as a compulsive behavior. The increased levels of signaling molecules found suggest that under this diet, the body no longer properly responds to the signaling pathway that regulates appetite. Most importantly, the observed change in gut microbiota composition not only supports previous studies, but its correlation with other results also points to how it can directly affect feeding behavior and brain signaling, thereby contributing to obesity. Researchers hope to further confirm this by transferring gut microbiota from HSB mice to normal mice and observing the effects. As specific species of gut microbiota that play critical roles in the development of obesity are identified, scientists may be able to design treatments that target these species to slow or prevent disease progression.
Featured Image Source: LJNovaScotia
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|