Trapping Sperm in Gel Could Lead to New Male Contraceptive
Contraceptives refer to methods or medical devices used to prevent pregnancy and allow for safer, healthier intercourse. They work in various ways to halt fertilization (the successful joining of an egg and sperm), thus avoiding pregnancy. Effective contraceptive methods also play a significant role in decreasing pregnancy-related morbidity and mortality rates and preventing the transmission of sexually transmitted diseases.
Current forms of medical contraception, however, are typically targeted towards females, such as birth control pills—hormonal medications designed to stop ovulation (the release of an egg)—or intrauterine devices (IUDs)—technology inserted into the uterus to prevent sperm from traveling effectively. However, besides condoms or spermicides, there are not as many options available for men. Additionally, contraceptives can fail; condoms have an average failure rate of 13% with typical use, while IUDs and medications are more effective at preventing pregnancy but are often less accessible and have potential side effects.
Therefore, researchers at Washington State University sought to investigate a potential contraceptive method for men. Normally in the male reproductive system, the organ known as the prostate holds seminal fluid, a mixture containing sperm. The “fluid” is initially stored as a gel due to semenogelins, or gel forming proteins. Semenogelins trap the sperm until it is released from the body through ejaculation, at which point an enzyme known as Prostate-Specific Antigen (PSA) breaks down the semenogelins to liquify semen. In its liquid form, the sperm can readily travel to an egg.
Using this information, scientists thought that as a solution to prevent fertilization, they could find a way to disrupt PSA’s function so that the seminal fluid remains a gel, leaving the sperm cells trapped.
Current forms of medical contraception, however, are typically targeted towards females, such as birth control pills—hormonal medications designed to stop ovulation (the release of an egg)—or intrauterine devices (IUDs)—technology inserted into the uterus to prevent sperm from traveling effectively. However, besides condoms or spermicides, there are not as many options available for men. Additionally, contraceptives can fail; condoms have an average failure rate of 13% with typical use, while IUDs and medications are more effective at preventing pregnancy but are often less accessible and have potential side effects.
Therefore, researchers at Washington State University sought to investigate a potential contraceptive method for men. Normally in the male reproductive system, the organ known as the prostate holds seminal fluid, a mixture containing sperm. The “fluid” is initially stored as a gel due to semenogelins, or gel forming proteins. Semenogelins trap the sperm until it is released from the body through ejaculation, at which point an enzyme known as Prostate-Specific Antigen (PSA) breaks down the semenogelins to liquify semen. In its liquid form, the sperm can readily travel to an egg.
Using this information, scientists thought that as a solution to prevent fertilization, they could find a way to disrupt PSA’s function so that the seminal fluid remains a gel, leaving the sperm cells trapped.
Image Source: sciencefreak
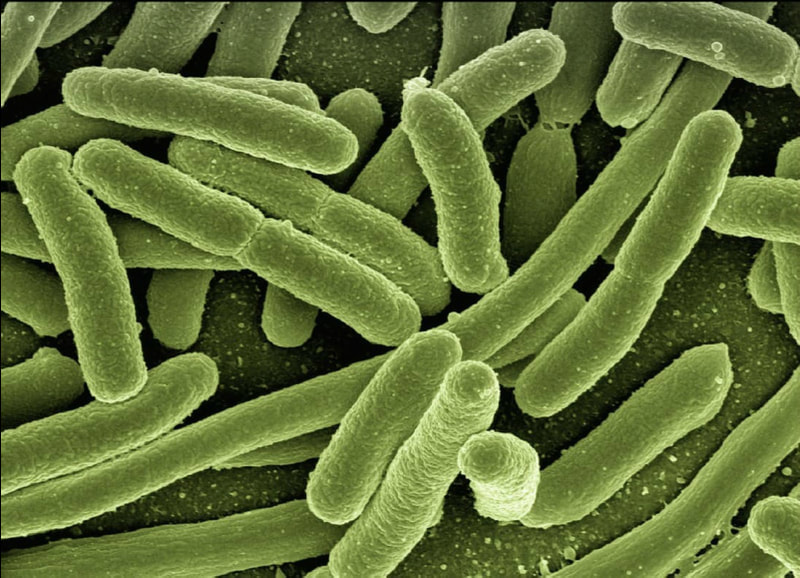
In a previous study, 4-2aminoethyl benzenesulfonyl fluoride(AEBSF), a molecule that blocks enzyme activity, prevented PSA function in mice which limited sperm’s ability to move. Researchers wondered if these results would apply to humans. Therefore, their research focused on AEBSF and an antibody (a type of immune system molecule that binds to molecules like PSA to disrupt them) to determine their effects on sperm mobility, semen viscosity (liquid thickness), and ability to disrupt PSA activity.
To measure sperm mobility, they gave different human semen samples either varying concentrations of AEBSF, a PSA-antibody, or a control group with neither of these. They then measured the samples via computer analysis to calculate how much the sperms’ movement has slowed down following treatment.
Finally, they measured the success of these molecules on disrupting PSA’s function. For AEBSF, they mixed treated samples with molecules that fluoresce in response to enzymatic activity. Since PSA is an enzyme, a decrease in light would indicate disrupted function.
The researchers discovered that the two highest concentrations of AEBSF increased semen liquid thickness by 309% and 463% respectively compared to the control group, while the top three concentrations limited sperm mobility. Meanwhile, the antibody also led to increased viscosity, but did not significantly reduce sperm mobility unlike AEBSF. These results are still exciting because limiting semen liquification has historically proven to cause infertility.
Nonetheless, these results are based on a single experiment and could be due to other factors. Since AEBSF is not specific to blocking just PSA, it is possible that it worked simply because of its toxicity, or because it disrupted other sperm-related enzymes. For the PSA antibody, a larger sample size or concentration could have been used to explain why it did not slow down sperm movement.
Despite these concerns, this study points to real potential for an efficient male contraceptive that will allow for fewer unexpected pregnancies and healthier intercourse. By altering sperm function, scientists are closer to expanding contraceptive options.
To measure sperm mobility, they gave different human semen samples either varying concentrations of AEBSF, a PSA-antibody, or a control group with neither of these. They then measured the samples via computer analysis to calculate how much the sperms’ movement has slowed down following treatment.
Finally, they measured the success of these molecules on disrupting PSA’s function. For AEBSF, they mixed treated samples with molecules that fluoresce in response to enzymatic activity. Since PSA is an enzyme, a decrease in light would indicate disrupted function.
The researchers discovered that the two highest concentrations of AEBSF increased semen liquid thickness by 309% and 463% respectively compared to the control group, while the top three concentrations limited sperm mobility. Meanwhile, the antibody also led to increased viscosity, but did not significantly reduce sperm mobility unlike AEBSF. These results are still exciting because limiting semen liquification has historically proven to cause infertility.
Nonetheless, these results are based on a single experiment and could be due to other factors. Since AEBSF is not specific to blocking just PSA, it is possible that it worked simply because of its toxicity, or because it disrupted other sperm-related enzymes. For the PSA antibody, a larger sample size or concentration could have been used to explain why it did not slow down sperm movement.
Despite these concerns, this study points to real potential for an efficient male contraceptive that will allow for fewer unexpected pregnancies and healthier intercourse. By altering sperm function, scientists are closer to expanding contraceptive options.
Featured Image Source: Clker-Free-Vector-Images
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|