The Gut Microbiota and Irritable Bowel Syndrome
Although there are approximately 100 trillion cells in the human body, only 10% are human cells – the other 90% are bacterial cells. Most of the bacteria are beneficial as they assist in food digestion, vitamin production, regulation of the immune system, and defense against harmful bacteria. Microorganisms, bacteria, viruses, and single-cell eukaryotes function together in the human body to create the human microbiome. Recently, researchers have turned their focus to the role played by these microbes in human health and well-being.
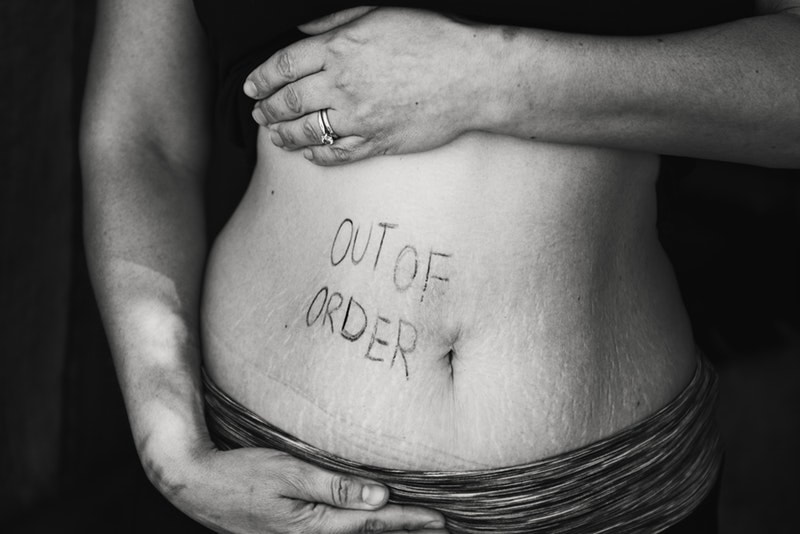
Irritable Bowel Syndrome (IBS), a gastrointestinal disorder characterized by cramping, abdominal pain, diarrhea or constipation, is a prevalent worldwide condition affecting 10% - 25% of the population in developed countries. IBS can be classified as IBS-D (diarrhea predominant), IBS-C (constipation predominant), IBS-M (mixed type), and IBS-U (unclassified). Although, the clear cause of IBS is not known, it has been speculated that IBS results from infection or overgrowth of bacteria in the intestines, inflammation in the intestines, and an imbalance in bacterial composition of the gut, also known as dysbiosis.
In order to better understand the pathogenesis of IBS, researchers from Protexin Probiotics have examined the role of gut bacteria, probiotics, and diet in IBS. Probiotics are substances which introduce beneficial bacterial species, such as those from the Lactobacillus and Bifidobacterium bacteria genera, to repopulate the gut with helpful bacteria. In turn, these beneficial bacteria can provide favorable effects including protection against harmful bacteria by taking up space and nutrient availability, regulation of immune responses, and production of neurotransmitting molecules that may participate in the gut-brain communication axis.
Irritable Bowel Syndrome (IBS), a gastrointestinal disorder characterized by cramping, abdominal pain, diarrhea or constipation, is a prevalent worldwide condition affecting 10% - 25% of the population in developed countries. IBS can be classified as IBS-D (diarrhea predominant), IBS-C (constipation predominant), IBS-M (mixed type), and IBS-U (unclassified). Although, the clear cause of IBS is not known, it has been speculated that IBS results from infection or overgrowth of bacteria in the intestines, inflammation in the intestines, and an imbalance in bacterial composition of the gut, also known as dysbiosis.
In order to better understand the pathogenesis of IBS, researchers from Protexin Probiotics have examined the role of gut bacteria, probiotics, and diet in IBS. Probiotics are substances which introduce beneficial bacterial species, such as those from the Lactobacillus and Bifidobacterium bacteria genera, to repopulate the gut with helpful bacteria. In turn, these beneficial bacteria can provide favorable effects including protection against harmful bacteria by taking up space and nutrient availability, regulation of immune responses, and production of neurotransmitting molecules that may participate in the gut-brain communication axis.
Image Source: Sponchia
Alternatively, prebiotics have been proposed as a treatment measure for IBS symptoms. Prebiotics are food ingredients that promote the growth of beneficial bacteria in the gut. These types of foods contain non-digestible dietary fibers, such as Inulin, Beta-glucan, or Fructooligosaccharides, which reach the colon after passing through the small intestine. The fibers then undergo fermentation, providing food for the favorable bacterial colonies. As a result, short chain fatty acids (SCFA) are produced as a byproduct. SCFA are known to offer anti-inflammatory, antitumorigenic and antimicrobial properties. Often times, both prebiotics and probiotics are used in conjunction, products known as synbiotics, to improve abdominal pain.
Recently, research has began investigating how diet affects the pathogenesis and remedial treatment of IBS. One study conducted by researchers at University of Sydney examined the efficacy of low FODMAP diet in ameliorating IBS symptoms. FODMAPS (fermentable oligo-, di-, monosaccharides and polyols) encompass a group of carbs including fructose, lactose, fructans, galactans and polyols. The basis for high FODMAP diet in IBS individuals is that not all of the digested food is absorbed by the small intestine. As a result, the unabsorbed residuals undergo bacterial fermentation leading to abdominal distension. Their analysis supports the notion that a low FODMAP diet is successful in reducing the severity of IBS symptoms. Although, the short-term use of low FODMAP diet has shown to reduce the severity of the symptoms, further studies are needed to investigate the long-term impact of this diet, which removes many nutrient-rich foods, on the microbiome.
These studies are budding ventures in discerning the relationship between the gut microbiome and IBS. However, further studies still need to be conducted in order to understand how the composition and metabolism of the microbiota interplays with the pathogenesis of IBS before more effective and efficient treatments can be developed to treat populations suffering from IBS.
Recently, research has began investigating how diet affects the pathogenesis and remedial treatment of IBS. One study conducted by researchers at University of Sydney examined the efficacy of low FODMAP diet in ameliorating IBS symptoms. FODMAPS (fermentable oligo-, di-, monosaccharides and polyols) encompass a group of carbs including fructose, lactose, fructans, galactans and polyols. The basis for high FODMAP diet in IBS individuals is that not all of the digested food is absorbed by the small intestine. As a result, the unabsorbed residuals undergo bacterial fermentation leading to abdominal distension. Their analysis supports the notion that a low FODMAP diet is successful in reducing the severity of IBS symptoms. Although, the short-term use of low FODMAP diet has shown to reduce the severity of the symptoms, further studies are needed to investigate the long-term impact of this diet, which removes many nutrient-rich foods, on the microbiome.
These studies are budding ventures in discerning the relationship between the gut microbiome and IBS. However, further studies still need to be conducted in order to understand how the composition and metabolism of the microbiota interplays with the pathogenesis of IBS before more effective and efficient treatments can be developed to treat populations suffering from IBS.
Featured Image Source: Kat Smith
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|