Rethinking the Alzheimer’s Diagnosis
Alzheimer’s disease is an irreversible, progressive disorder that causes dementia symptoms to worsen over time and brain cells to degenerate and eventually die. In its early stages, Alzheimer's patients experience mild memory loss and a decline in thinking, behavioural and social skills, leading to a completely dependent lifestyle. Later stages involve severe memory impairment, including the inability to carry out a conversation and other everyday tasks.
Alzheimer’s was originally listed as the sixth-leading cause of death by the Centers for Disease Control and Prevention (CDC). However, a Neurology report published in 2014 suggests that the current procedure for determining Alzheimer-related deaths (using death certificates) downplays the severity and impact of Alzheimer’s. Originally, the CDC linked 84,000 deaths in 2010 to Alzheimer’s disease, but the 2014 report predicted the number to be closer to 503,400 among people ages 75 and over, thus placing Alzheimer’s third among leading causes of death, behind heart disease and cancer.
Previously, characteristic plaques and tangles were detectable only through autopsies, meaning doctors were unable to definitively diagnose Alzheimer’s among living patients—they could only take note of common symptoms such as progressive memory loss and cognitive decline. Since dementia could be associated with multiple brain disorders, such as frontotemporal disorders or vascular brain injury, health care providers cannot conclude the activity of Alzheimer’s through dementia symptoms.
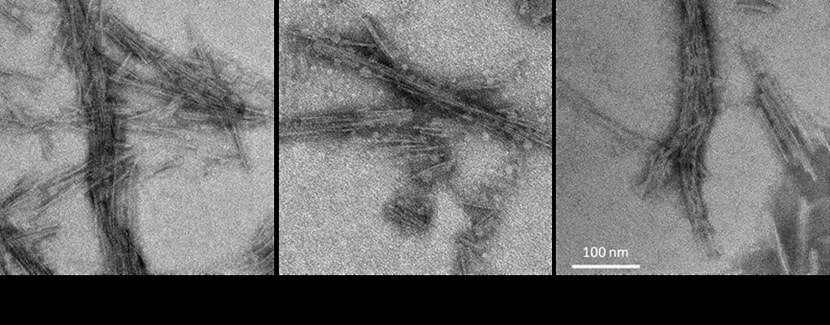
Alzheimer’s is defined through the buildup of amyloid protein plaques around nerve cells and the tangles of tau protein within cells. By imaging disease brains, Mayo Clinic neuroradiologists concluded that the cognitive symptoms attributed to the disease are related to the tau protein tangles. Tau is not commonly observed in the brain unless amyloid is present. Thus, they reasoned that the role of amyloid is to enable the spread of tau. Though it is uncertain whether dementia is purely the result of the buildup of amyloid and tau, scientists are confident that the presence of plaques and tangles, which increase in frequency as subjects age, translates to a variety of brain changes that precede dementia.
Alzheimer’s was originally listed as the sixth-leading cause of death by the Centers for Disease Control and Prevention (CDC). However, a Neurology report published in 2014 suggests that the current procedure for determining Alzheimer-related deaths (using death certificates) downplays the severity and impact of Alzheimer’s. Originally, the CDC linked 84,000 deaths in 2010 to Alzheimer’s disease, but the 2014 report predicted the number to be closer to 503,400 among people ages 75 and over, thus placing Alzheimer’s third among leading causes of death, behind heart disease and cancer.
Previously, characteristic plaques and tangles were detectable only through autopsies, meaning doctors were unable to definitively diagnose Alzheimer’s among living patients—they could only take note of common symptoms such as progressive memory loss and cognitive decline. Since dementia could be associated with multiple brain disorders, such as frontotemporal disorders or vascular brain injury, health care providers cannot conclude the activity of Alzheimer’s through dementia symptoms.
Alzheimer’s is defined through the buildup of amyloid protein plaques around nerve cells and the tangles of tau protein within cells. By imaging disease brains, Mayo Clinic neuroradiologists concluded that the cognitive symptoms attributed to the disease are related to the tau protein tangles. Tau is not commonly observed in the brain unless amyloid is present. Thus, they reasoned that the role of amyloid is to enable the spread of tau. Though it is uncertain whether dementia is purely the result of the buildup of amyloid and tau, scientists are confident that the presence of plaques and tangles, which increase in frequency as subjects age, translates to a variety of brain changes that precede dementia.
Image Source: Samples of cerebrospinal fluid used to detect tauopathies by NIH Image Gallery
is licensed under Public Domain Mark 1.0
is licensed under Public Domain Mark 1.0
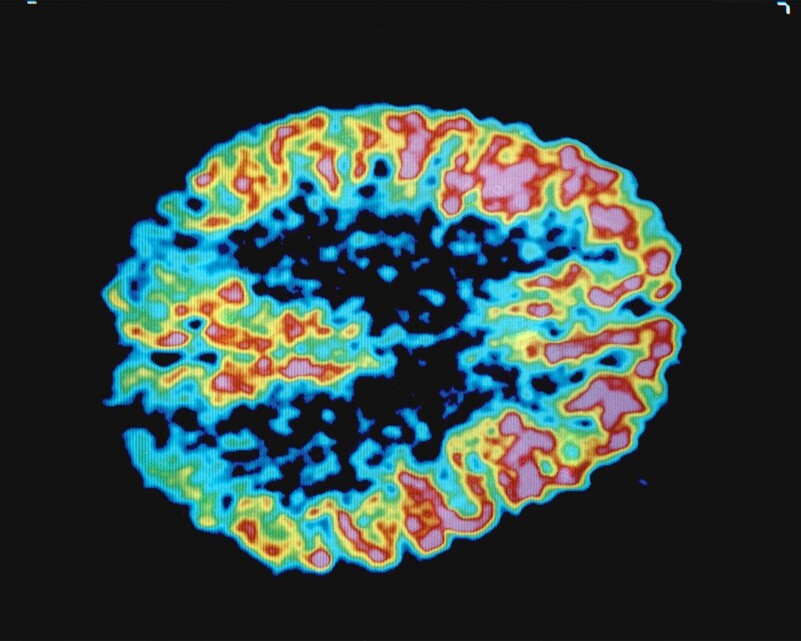
Researchers at the Mayo Clinic’s Disease Research Center have begun using imaging to study brain changes among suspected Alzheimer’s patients. Previously, the diagnosis of Alzheimer’s hinged on identifying dementia; Alzheimer’s key symptom. Yet, they suspected a gradual progression of brain changes that precede dementia including memory loss or behavioural symptoms.
The researchers established that Alzheimer’s disease first surfaces as amyloid plaques in a healthy brain with normal, unaltered cognition. Gradually, a patient will show symptoms of mild cognitive impairment before eventually experiencing dementia. Thus, they suggested Alzheimer’s be characterized by its underlying biology—plaque buildup—and not through dementia symptoms that arise as a common side effect.
This new definition for Alzheimer's diagnosis changes how we approach treatment. First, it concludes that more people have Alzheimer’s than previously predicted. Now, in addition to the 5.5 million Americans diagnosed with Alzheimer’s every year, there could potentially be over 10 million more with plaques and tau tangles who show no outward symptoms or cognitive impairment. Modification of the diagnostic criteria also advances the possibilities for researchers to detect early stages of the disease and trace the spread of the plaque and tangles in patients. Health care specialists will also be able to target new drugs on altering the progression of plaques and tangles.
The researchers established that Alzheimer’s disease first surfaces as amyloid plaques in a healthy brain with normal, unaltered cognition. Gradually, a patient will show symptoms of mild cognitive impairment before eventually experiencing dementia. Thus, they suggested Alzheimer’s be characterized by its underlying biology—plaque buildup—and not through dementia symptoms that arise as a common side effect.
This new definition for Alzheimer's diagnosis changes how we approach treatment. First, it concludes that more people have Alzheimer’s than previously predicted. Now, in addition to the 5.5 million Americans diagnosed with Alzheimer’s every year, there could potentially be over 10 million more with plaques and tau tangles who show no outward symptoms or cognitive impairment. Modification of the diagnostic criteria also advances the possibilities for researchers to detect early stages of the disease and trace the spread of the plaque and tangles in patients. Health care specialists will also be able to target new drugs on altering the progression of plaques and tangles.
Featured Image Source: 194 001 001 by U.S. Department of Energy is a licensed United States government work
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|