Plastic Replaced: New Bioengineering Solutions for Dialysis
Chronic kidney disease (CKD) is a common long-term medical condition affecting 37 million people in the United States and looming over millions of at-risk others. People with this disease have impaired kidneys, the organs in charge of filtering blood and excreting waste as urine, that gradually lose function over time. As a result, this leads to a buildup of waste in the blood and can cause a person to feel sick with symptoms including anemia, sleeping problems, high blood pressure, and nerve damage. Unfortunately, there is no complete cure for CKD, and most treatments focus on slowing the rate of kidney failure itself. Once CKD progresses to end-stage renal disease (ESRD), where the kidney is only working at 10-15% of its normal function, patients are confronted with only two options: a kidney transplant or kidney dialysis.
Hemodialysis is the most common type of dialysis and involves routing blood from the body into an artificial “kidney” machine that cleans and filters the blood before returning it back to the body. To access the blood, an artery and a vein are fused together to make a fistula, from which blood is exchanged. However, for patients whose blood vessels are not strong enough to form a fistula, a grafted soft plastic prosthetic tube is often used. This tube presents new risks, including triggering the patient’s immune response and inducing blood clots. To solve this issue, scientists at both Duke and Yale University have bioengineered a new solution: human acellular vessels (HAV).
Hemodialysis is the most common type of dialysis and involves routing blood from the body into an artificial “kidney” machine that cleans and filters the blood before returning it back to the body. To access the blood, an artery and a vein are fused together to make a fistula, from which blood is exchanged. However, for patients whose blood vessels are not strong enough to form a fistula, a grafted soft plastic prosthetic tube is often used. This tube presents new risks, including triggering the patient’s immune response and inducing blood clots. To solve this issue, scientists at both Duke and Yale University have bioengineered a new solution: human acellular vessels (HAV).
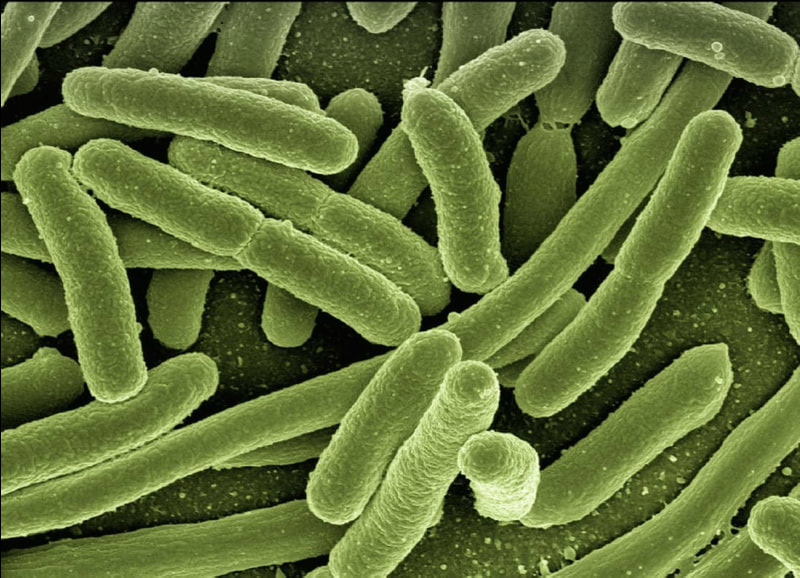
Human acellular vessels, as explained in their new study, are artificial vessels created from the human extracellular matrix (ECM), the material that surrounds cells in body tissues. The researchers were able to fabricate the vessels by creating a skeleton of biodegradable mesh and embedding human vessel cells into the mesh. Following 8 weeks of growth, the cells expanded to create a basic ECM around themselves. To prevent immune detection, these cells were then removed and the scaffold degraded, leaving only the vessel-shaped ECM behind.
To support clinical implementation, the researchers sought to better understand if the vessels were likely an acceptable alternative to traditional plastic tubing for grant implantation. To do so, 60 patients suffering from ESRD received HAV implants in their arms. 13 of these were later removed due to various medical complications, while the remaining 47 HAV implants functioned satisfactorily. When examining the grafts removed, researchers noticed something interesting–the ECM of the HAV were becoming populated by the host’s own cells. This suggests that implants of HAV can eventually be repurposed by the body to become living vessels.
While this invention is still in its fourth year of clinical trials, the discoveries uncovered are promising. This research gives patients who need alternatives to the standard plastic grafts in hemodialysis more hope in their recovery processes. In addition, it also provides a possible method of engineering the body to make the graft itself, a completely new realm of research not considered before. With further work, bioengineering in this aspect could be expanded into a variety of potential treatment options for other diseases and help deliver a better quality of life to many.
To support clinical implementation, the researchers sought to better understand if the vessels were likely an acceptable alternative to traditional plastic tubing for grant implantation. To do so, 60 patients suffering from ESRD received HAV implants in their arms. 13 of these were later removed due to various medical complications, while the remaining 47 HAV implants functioned satisfactorily. When examining the grafts removed, researchers noticed something interesting–the ECM of the HAV were becoming populated by the host’s own cells. This suggests that implants of HAV can eventually be repurposed by the body to become living vessels.
While this invention is still in its fourth year of clinical trials, the discoveries uncovered are promising. This research gives patients who need alternatives to the standard plastic grafts in hemodialysis more hope in their recovery processes. In addition, it also provides a possible method of engineering the body to make the graft itself, a completely new realm of research not considered before. With further work, bioengineering in this aspect could be expanded into a variety of potential treatment options for other diseases and help deliver a better quality of life to many.
Featured Image Source: geralt
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|