New Stem Cell Technology Shows Promising Progress for Neurodegenerative Diseases and Developmental Disorders
Nearly 6.5 million people harbor neurodegenerative diseases, which inhibit normal function of the spinal cord, nervous system, and brain. Furthermore, the Center for Disease Control and Prevention (CDC) stated that as of 2015, nearly 15% of children ages 3-17 suffer from either one or more developmental disorders (ex. Autism Spectrum Disorder (ASD)). If active solutions and treatments for these diseases and disorders cannot be found, the number of those affected will only continue to rise.
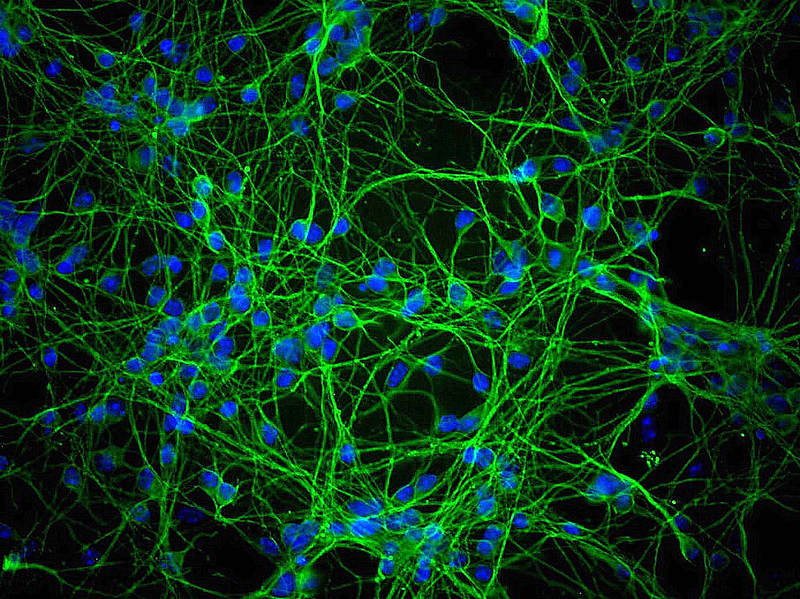
Why haven’t scientists made significant progress yet? The problem is the lack of healthy and diseased brain tissue scientists have access to in order to perform clinical trials and experiments on; in addition, it is extremely difficult to grow, cultivate, and manipulate this tissue. This problem has forced scientists to look toward the future of generating new cells from pre-existing adult cells using a technique known as induced pluripotent stem cell technology (iPSC technology). Human pluripotent stem cells (hPSCs) derived from iPSCs in humans can be used to create 3D models of neurodegenerative diseases and developmental disorders to further research and progress on developing treatments.
This research used 3D brain organoids, mini organs that are cultivated from hPSCs to look and act like the brain for modeling and experimental purposes. In this research, autosomal recessive primary microcephaly (MCPH), a disease known for shrinking the size of the brain, was studied. 3D brain organoids that were injected into mice did not show a significantly reduced brain size. iPSCs were then taken from these injected mice, and when compared to iPSCs made from a patient with MCPH, the patient-made iPSCs were found to have a smaller brain size, altered cell orientation, and an abundance of neuron outgrowth. The use of 3D brain organoids to show the small change in brain size on mice injected with MCPH allowed for researchers to understand that mice do not experience MCPH as severely as humans do.
Next, the research shifted focus to using 3D brain organoids to study the Zika virus, a recent world epidemic affecting pregnant woman. When scientists use 3D hPSCs cerebral organoids to model the effects of the virus, they found an overall decrease in organoid size, embryonic tissue, and cortical plate thickness (a layer of compact bone). Further analysis of these organoids lead to the discovery of potential genes that could cause cells to die and impact neural growth. This technology could be used to model other viruses and discover potential genes that influence viruses. The use of 3D cerebral organoids has given researchers a better understanding of the effects of Zika and ability to treat the virus since they could pinpoint areas of focus where treatment is required.
Why haven’t scientists made significant progress yet? The problem is the lack of healthy and diseased brain tissue scientists have access to in order to perform clinical trials and experiments on; in addition, it is extremely difficult to grow, cultivate, and manipulate this tissue. This problem has forced scientists to look toward the future of generating new cells from pre-existing adult cells using a technique known as induced pluripotent stem cell technology (iPSC technology). Human pluripotent stem cells (hPSCs) derived from iPSCs in humans can be used to create 3D models of neurodegenerative diseases and developmental disorders to further research and progress on developing treatments.
This research used 3D brain organoids, mini organs that are cultivated from hPSCs to look and act like the brain for modeling and experimental purposes. In this research, autosomal recessive primary microcephaly (MCPH), a disease known for shrinking the size of the brain, was studied. 3D brain organoids that were injected into mice did not show a significantly reduced brain size. iPSCs were then taken from these injected mice, and when compared to iPSCs made from a patient with MCPH, the patient-made iPSCs were found to have a smaller brain size, altered cell orientation, and an abundance of neuron outgrowth. The use of 3D brain organoids to show the small change in brain size on mice injected with MCPH allowed for researchers to understand that mice do not experience MCPH as severely as humans do.
Next, the research shifted focus to using 3D brain organoids to study the Zika virus, a recent world epidemic affecting pregnant woman. When scientists use 3D hPSCs cerebral organoids to model the effects of the virus, they found an overall decrease in organoid size, embryonic tissue, and cortical plate thickness (a layer of compact bone). Further analysis of these organoids lead to the discovery of potential genes that could cause cells to die and impact neural growth. This technology could be used to model other viruses and discover potential genes that influence viruses. The use of 3D cerebral organoids has given researchers a better understanding of the effects of Zika and ability to treat the virus since they could pinpoint areas of focus where treatment is required.
Image Source: "Encontro Apoio Juridico Movimento Zika - 02/09/2017" by Central Produções is licensed under CC BY-NC-SA 2.0
Lastly, scientists used iPSC technology when studying Autism Spectrum Disorder (ASD). Using iPSC technology, researchers saw that genetic variations in autistic patients who exhibited a large number of hPSCs created from neural cells showed an increase in gene variation at later stages of cultivating hPSCs. The use of iPSC technology showed the genetic level of causation of ASD that scientists were unable to study before. These findings help enforce the idea that signaling between neurons plays a huge role in ASD and that enhancing iPSC technology and organoids could further research into the disorder.
The success of 3D brain organoids in neurodegenerative diseases and developmental disorders being able to pinpoint specific problematic genes, see differences in genetic variation on a deeper level, and model the changes in brain size for comparison has become a gateway for further application of this technology to study other diseases and disorders. Progress has been made by 3D brain organoids to understand the causations and effects better for MCPH, Zika virus, and ASD that can now help doctors more effectively treat changes that occur in their affected patient’s bodies. As scientists are currently looking toward the innovation of hiSPCs for personalized cell replacement therapy, the success and potential of using 3D brain organoids with iSPC technology give hope for those affected by these neurodegenerative diseases and developmental disorders around the world.
The success of 3D brain organoids in neurodegenerative diseases and developmental disorders being able to pinpoint specific problematic genes, see differences in genetic variation on a deeper level, and model the changes in brain size for comparison has become a gateway for further application of this technology to study other diseases and disorders. Progress has been made by 3D brain organoids to understand the causations and effects better for MCPH, Zika virus, and ASD that can now help doctors more effectively treat changes that occur in their affected patient’s bodies. As scientists are currently looking toward the innovation of hiSPCs for personalized cell replacement therapy, the success and potential of using 3D brain organoids with iSPC technology give hope for those affected by these neurodegenerative diseases and developmental disorders around the world.
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|