New Insights on the Tau Protein in Treating Alzheimer's Disease
Between 60% and 80% of dementia cases are attributed to Alzheimer’s disease (AD), a neurological condition that progressively destroys memory, cognition, and eventually the ability to carry out everyday tasks. Currently, there is no monotherapeutic cure for the condition. Alzheimer’s patients are often prescribed a combination of cognition-enhancing medications and lifestyle changes, such as frequent aerobic exercise and a Mediterranean diet, which can slow the disease. Nonetheless, the number of adults over 65 (the group most at risk for AD) is expected to double within the next 40 years, calling for more effective, accessible, and affordable treatment.
A novel study from the University of California, Riverside (UCR) pinpointed the key difference in brain composition between people who developed Alzheimer’s and those who didn’t. Researchers studied different forms of a protein called tau, found abundantly in neurons in the brain. Abnormal tau proteins are believed to contribute to the development of AD, making them an ideal target for clinical research.
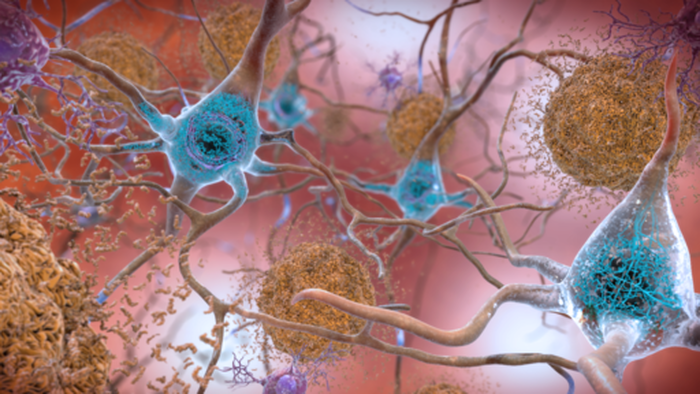
The study investigated how tau contributes to the development of plaques and tangles, two hallmark indicators of Alzheimer’s. Plaques are abnormal clusters of protein pieces, while tangles are knots of dead and dying brain cells. These buildups block communication between neurons in the brain, causing the decline in cognition observed in AD.
The researchers analyzed the molecular composition of donated brain samples from deceased subjects. Interestingly, they found that over 20% of subjects had plaques and tangles but no signs of dementia. This caused speculation over whether the plaques and tangles themselves were truly the cause of the disease, leading to an even more dramatic discovery: only those who developed plaques and tangles and had an alternate form of tau developed AD.
A novel study from the University of California, Riverside (UCR) pinpointed the key difference in brain composition between people who developed Alzheimer’s and those who didn’t. Researchers studied different forms of a protein called tau, found abundantly in neurons in the brain. Abnormal tau proteins are believed to contribute to the development of AD, making them an ideal target for clinical research.
The study investigated how tau contributes to the development of plaques and tangles, two hallmark indicators of Alzheimer’s. Plaques are abnormal clusters of protein pieces, while tangles are knots of dead and dying brain cells. These buildups block communication between neurons in the brain, causing the decline in cognition observed in AD.
The researchers analyzed the molecular composition of donated brain samples from deceased subjects. Interestingly, they found that over 20% of subjects had plaques and tangles but no signs of dementia. This caused speculation over whether the plaques and tangles themselves were truly the cause of the disease, leading to an even more dramatic discovery: only those who developed plaques and tangles and had an alternate form of tau developed AD.
Image Source: "Beta-Amyloid Plaques and Tau in the Brain" by NIH Image Gallery is licensed under the public domain
So what’s the significance of tau? Proteins like tau are made up of smaller units called amino acids. Like the preferential use of one hand in humans, these amino acids can take on either right-handed or left-handed forms called isomers. Normally, proteins in living things are made mainly from “left-handed” amino acids. However, if proteins last for too long, their amino acids can turn into “right-handed” isomers. Using a right-handed isomer is similar to putting a right-handed glove on a left hand: it simply doesn’t fit. Thus, an accumulation of proteins made of right-handed isomers in the brain can lead to serious problems.
But how does this problem arise in the first place? Normally, the human body clears itself of defective proteins through a process called autophagy. Literally meaning “self-eating,” autophagy is like a molecular garbage recycling system, clearing the body of unnecessary or damaged cellular components. Unfortunately, as an individual ages, autophagy slows down, causing dysfunctional proteins to accumulate in the body. This slowing is partly why AD is most prominent in those over 65.
Although it is not entirely understood why autophagy slows with age, this new understanding of tau isomers could give rise to more effective treatments. According to the UCR researchers, autophagy can be promoted by fasting and exercising. When cells run out of proteins obtained via one’s diet, they begin to break down existing proteins. As a result, old proteins are recycled and the body is cleared of cellular waste. Thus, lifestyle modifications can be important components of an AD treatment plan.
This new insight has also led to the development of drugs designed to improve the process of autophagy. In addition, several existing drugs that optimize autophagy for conditions like cardiovascular diseases may soon be approved for neurodegenerative diseases such as Alzheimer’s disease. Perhaps the solution to one of the most debilitating diseases in the world has been underneath our noses all along.
But how does this problem arise in the first place? Normally, the human body clears itself of defective proteins through a process called autophagy. Literally meaning “self-eating,” autophagy is like a molecular garbage recycling system, clearing the body of unnecessary or damaged cellular components. Unfortunately, as an individual ages, autophagy slows down, causing dysfunctional proteins to accumulate in the body. This slowing is partly why AD is most prominent in those over 65.
Although it is not entirely understood why autophagy slows with age, this new understanding of tau isomers could give rise to more effective treatments. According to the UCR researchers, autophagy can be promoted by fasting and exercising. When cells run out of proteins obtained via one’s diet, they begin to break down existing proteins. As a result, old proteins are recycled and the body is cleared of cellular waste. Thus, lifestyle modifications can be important components of an AD treatment plan.
This new insight has also led to the development of drugs designed to improve the process of autophagy. In addition, several existing drugs that optimize autophagy for conditions like cardiovascular diseases may soon be approved for neurodegenerative diseases such as Alzheimer’s disease. Perhaps the solution to one of the most debilitating diseases in the world has been underneath our noses all along.
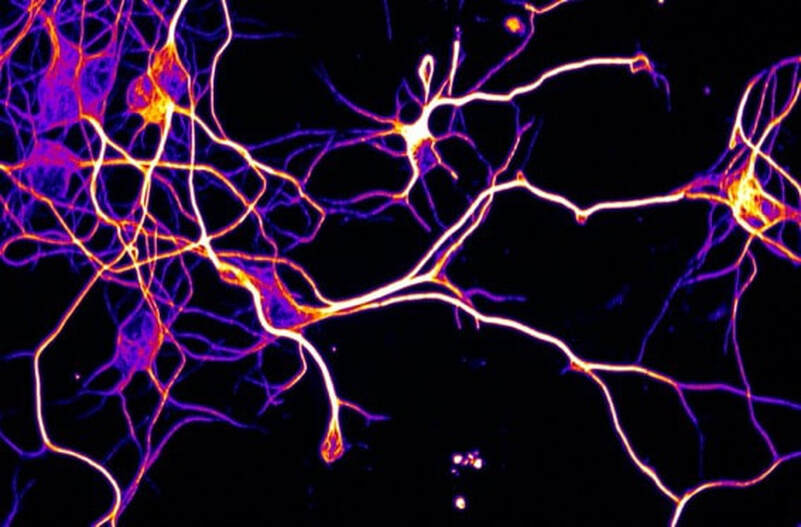
Featured Image Source: "Axons from an Alzheimer's mouse model" by Brian6122 is licensed under CC BY 4.0
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|