Low Antibiotics Doses May Lead to High Antibiotic Resistance
Since the discovery of antibiotics in the 1920s, common medical practice uses antibiotics to treat bacterial infections. However, the increased antibiotic usage for treating bacterial infections has led to the development of antibiotic resistance in bacteria. Antibiotic resistance, therefore, has become a primary concern of public health. A recent study by Upssala University in Sweden found that small amounts of antibiotics in bacterial environments can lead to the development of high antibiotic resistance.
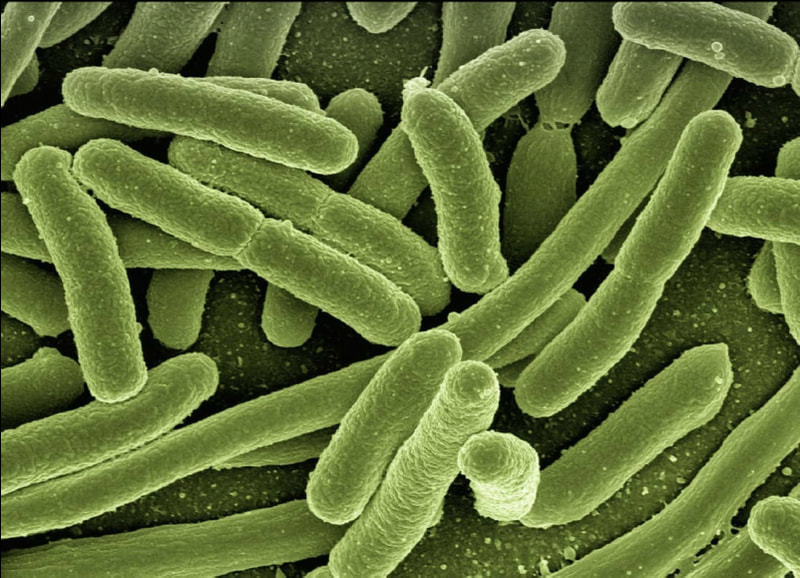
Antibiotic resistance is a phenomenon in which the bacteria adapt to the antibiotic, so it loses the ability to kill bacteria or its growth. The bacteria that survived often contain mutations within their genes that give the bacteria antibiotic resistance. As a result, the antibiotics used to treat bacteria infection has a potential risk of developing antibiotic resistance in the bacteria that are able to survive the dose of antibiotics.
Antibiotic resistance is a phenomenon in which the bacteria adapt to the antibiotic, so it loses the ability to kill bacteria or its growth. The bacteria that survived often contain mutations within their genes that give the bacteria antibiotic resistance. As a result, the antibiotics used to treat bacteria infection has a potential risk of developing antibiotic resistance in the bacteria that are able to survive the dose of antibiotics.
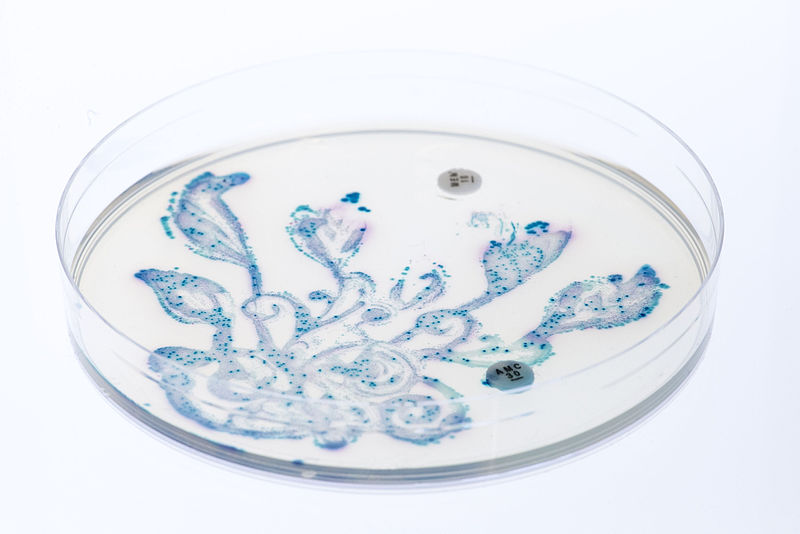
Image Source: sbtlneet
Previous studies have shown that antibiotic doses above the minimal inhibitory concentration (MIC), high antibiotic cross resistance develops rapidly; however, little is known about the small antibiotic doses and its potential in developing antibiotic resistance. This is crucial for the current medical practice as antibiotics are often used to treat bacterial infections in humans or, even, promote growth in livestocks. As a result of these anthropogenic factors, small doses of antibiotics are often released into the environment. To shed light on the effect of prolonged treatment of small doses of antibiotics (below MIC) on the bacteria, the researchers in the Uppsala University worked with the bacteria Salmonella enterica. 900 generations of wild-type streptomycin susceptible S. enterica were passed through streptomycin, reducing the growth rate of the bacteria by 3%, which allowed the researchers to select bacterial colonies for their sub-MIC (below MIC) experiment. After obtaining the bacterial colonies, these bacteria were treated with different doses of streptomycin. The researchers found that within the bacterial colonies that underwent prolonged small dose treatment, several sub-colonies of bacteria possessed high antibiotic resistance. The research concluded that under high dose selection, the susceptible bacteria would stop growing or die, but at low doses (sub-MIC), the bacteria will still grow while they are under selection of the antibiotic, generating an increase in resistance through the accumulation of resistant mutations.
Overall, the implication of this study highlights the potential threat that antibiotics can impose by promoting antibiotic resistance. Therefore, it is crucial to understand how antibiotic resistance is developed and to be mindful of the use of antibiotics.
Overall, the implication of this study highlights the potential threat that antibiotics can impose by promoting antibiotic resistance. Therefore, it is crucial to understand how antibiotic resistance is developed and to be mindful of the use of antibiotics.
Featured Image Source: PublicDomainPictures
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|