IspH Inhibtors: The Cure to Antimicrobial Resistance?
The race against antimicrobial resistance has left the future of science and medicine looking bleak. Within the past century, the rise in the use of antibiotics, or drugs that target and kill certain bacteria, has in turn produced resistant bacteria and rendered many modern antibiotics ineffective. However, the recent discovery of a new class of antibiotics has sparked hope for the future of medicine and health.
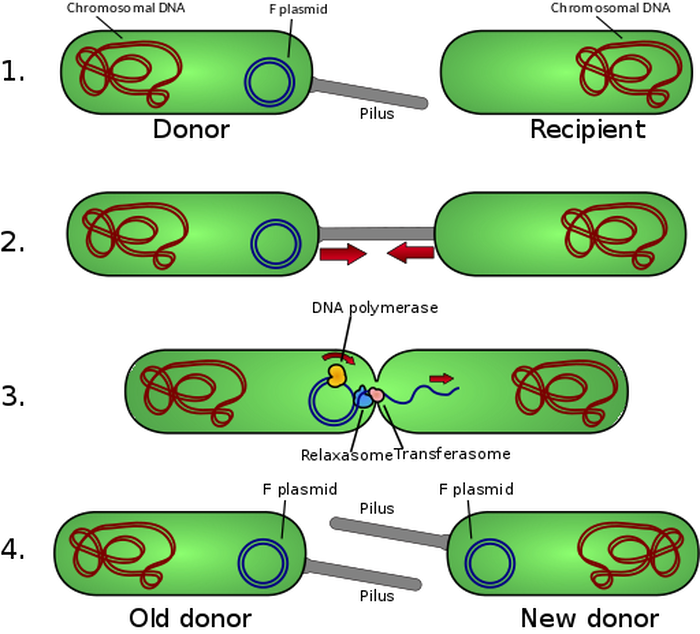
Antibiotic use dates back to the early 1930’s. Alexander Fleming’s discovery of penicillin in 1928 led to its establishment as a worldwide “wonder drug,” prescribed to treat everything from strep throat to syphilis. However, the mass consumption of antibiotics has led to an epidemic of antimicrobial resistance (AMR). Over time, bacteria have found novel ways to survive, including changing the target for the antibiotic, pumping the drug out, and limiting the pathways through which the drug can enter, to name a few. Another difficulty is that resistance genes can be transferred across different bacteria through a process called horizontal gene transfer, meaning that resistance to antibiotics can spread rapidly through the environment. AMR is a global health emergency: around 700,000 lives are claimed each year by infections that are not curable with current antibiotics, and many antibiotics that used to be powerful in treating infectious disease are now entirely ineffective.
The discovery of a new class of antibiotics, however, has the potential to save the hundreds of thousands of lives affected by AMR. These prodrugs are called IspH inhibitors, meaning they work to specifically block the activity of the enzyme IspH. IspH is an important enzyme in a biochemical process called the methyl erythritol phosphate pathway in bacteria, which creates molecules called isoprenoids. Isoprenoids are essential to the survival of pathogenic (disease-causing) bacteria, supporting their stability and overall function. IspH inhibitors target the IspH enzyme in order to block the entire pathway altogether and kill microbes.
Antibiotic use dates back to the early 1930’s. Alexander Fleming’s discovery of penicillin in 1928 led to its establishment as a worldwide “wonder drug,” prescribed to treat everything from strep throat to syphilis. However, the mass consumption of antibiotics has led to an epidemic of antimicrobial resistance (AMR). Over time, bacteria have found novel ways to survive, including changing the target for the antibiotic, pumping the drug out, and limiting the pathways through which the drug can enter, to name a few. Another difficulty is that resistance genes can be transferred across different bacteria through a process called horizontal gene transfer, meaning that resistance to antibiotics can spread rapidly through the environment. AMR is a global health emergency: around 700,000 lives are claimed each year by infections that are not curable with current antibiotics, and many antibiotics that used to be powerful in treating infectious disease are now entirely ineffective.
The discovery of a new class of antibiotics, however, has the potential to save the hundreds of thousands of lives affected by AMR. These prodrugs are called IspH inhibitors, meaning they work to specifically block the activity of the enzyme IspH. IspH is an important enzyme in a biochemical process called the methyl erythritol phosphate pathway in bacteria, which creates molecules called isoprenoids. Isoprenoids are essential to the survival of pathogenic (disease-causing) bacteria, supporting their stability and overall function. IspH inhibitors target the IspH enzyme in order to block the entire pathway altogether and kill microbes.
IspH inhibitors as a whole are not new to the world of antibiotics—old forms of these drugs could not penetrate the bacterial cell wall. By contrast, in addition to being able to probe inside the bacterial cells, the new class of IspH inhibitors activates the human immune system, specifically targeting T cells. This immune system activation is key to the efficacy behind this new class of antibiotics, working as a secondary attack on the bacteria. This combination leads to an extremely successful drug, with models so far showing it to be more effective than traditional antibiotics of the past.
Researchers used a multipronged strategy to test the prodrugs; they purified IspH proteins from various bacterial species, calculated the optimal concentrations and reaction time of IspH, and then performed a molecular docking study using IspH from E. coli bacteria to predict how the protein interacts with other molecules. Using computer modeling, they screened millions of commercial compounds for their ability to bind with IspH, selecting the ones that inhibited the enzyme most effectively, and then modified those compounds into prodrugs for delivery into bacterial cells. It was shown that these IspH inhibitors killed off multi-drug resistant bacteria that are unscathed by current antibiotics. Additionally, the inhibitors are relatively non-toxic to the cells of mammals, an important requirement for antibiotics to reach the market.
This advance does not necessarily mean that AMR is cured. It is still critical that we monitor and regulate our antibiotic use to ensure that bacteria do not quickly become resistant again. Yet, this new discovery surely makes the future seem less bleak.
Researchers used a multipronged strategy to test the prodrugs; they purified IspH proteins from various bacterial species, calculated the optimal concentrations and reaction time of IspH, and then performed a molecular docking study using IspH from E. coli bacteria to predict how the protein interacts with other molecules. Using computer modeling, they screened millions of commercial compounds for their ability to bind with IspH, selecting the ones that inhibited the enzyme most effectively, and then modified those compounds into prodrugs for delivery into bacterial cells. It was shown that these IspH inhibitors killed off multi-drug resistant bacteria that are unscathed by current antibiotics. Additionally, the inhibitors are relatively non-toxic to the cells of mammals, an important requirement for antibiotics to reach the market.
This advance does not necessarily mean that AMR is cured. It is still critical that we monitor and regulate our antibiotic use to ensure that bacteria do not quickly become resistant again. Yet, this new discovery surely makes the future seem less bleak.
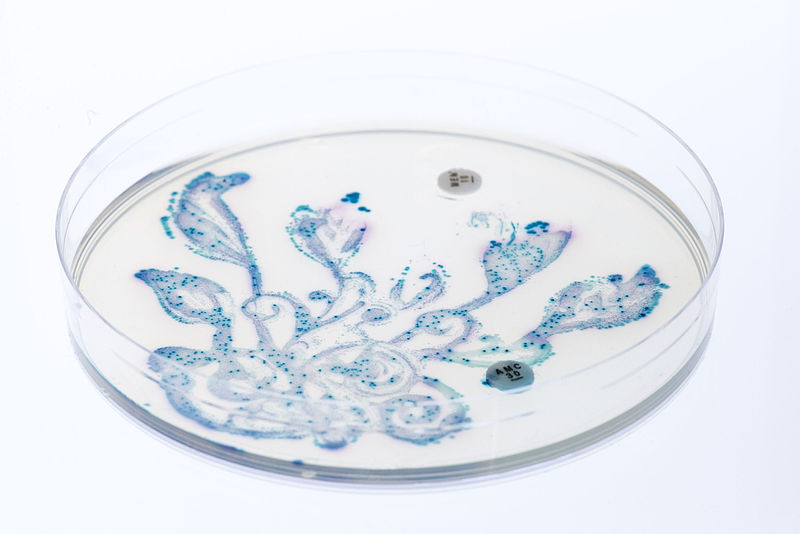
Featured Image Source: Polina Tankilevitch
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|