Hearts Revived: Avoiding Permanent Injury From Heart Attacks
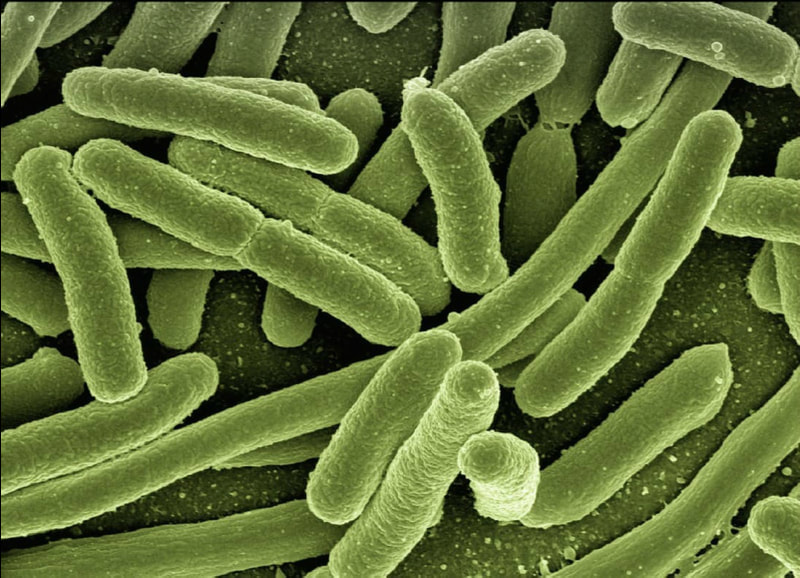
Myocardial infarctions, otherwise known as heart attacks, affect approximately 805,000 Americans every year, with one occurring every 40 seconds within the United States. Heart attacks stem from plaque buildup in the coronary arteries, vessels that supply blood to the heart muscle (myocardium). Breakage of the buildup initiates blood clot formation at the site, which in turn causes ischemia, a lack of oxygen and blood flow to body tissues. The resulting death of myocardial tissue due to that lack of oxygen is referred to as a myocardial infarction. Although getting blood flow back to the affected tissue is the ideal method of treatment for myocardial infarctions, this may result in an even greater extent of tissue damage known as ischemia-reperfusion injury (IRI). Today, progress in effective therapies for heart attacks is hindered because of the complexities of IRI.
Currently, a procedure called ischemic preconditioning has been proven to protect against this cardiac stress, but only experimentally in animal species and in vitro settings (culture dish experiments). As described by its name, ischemic preconditioning involves inducing short periods of ischemia followed by short periods of reperfusion, or restoration of blood flow—essentially “conditioning” the heart as an athlete would before a match—before a prolonged period of ischemia. This method has been observed to reduce the amount of injury to tissue.
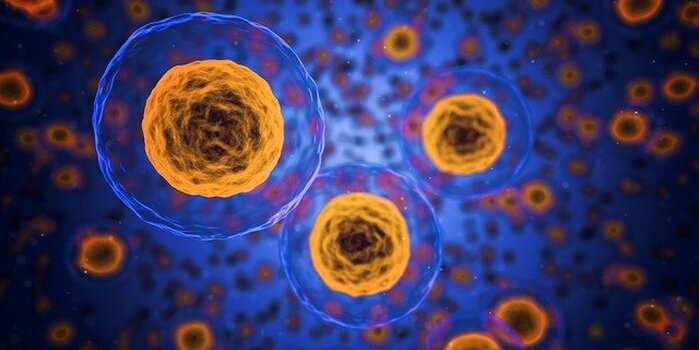
Another method of reducing tissue injury caused by ischemia uses vascular endothelial cells, which are located in the inner lining of blood vessels. Their extracellular vesicles (EVs), which are small membrane-enclosed components released from the cell, are key to the treatment, but it was unclear exactly how these vesicles function. Harvard University researchers hypothesized that these endothelial extracellular vesicles (EEVs) hold the potential to produce a protective effect on cardiac tissue by acting as messengers to other cells. The researchers mapped all the proteins found in EEVs and discovered specific protein groups that are also present during ischemic preconditioning. They concluded that this similarity signifies these protein groups have an important role in protecting cardiac tissue.
Currently, a procedure called ischemic preconditioning has been proven to protect against this cardiac stress, but only experimentally in animal species and in vitro settings (culture dish experiments). As described by its name, ischemic preconditioning involves inducing short periods of ischemia followed by short periods of reperfusion, or restoration of blood flow—essentially “conditioning” the heart as an athlete would before a match—before a prolonged period of ischemia. This method has been observed to reduce the amount of injury to tissue.
Another method of reducing tissue injury caused by ischemia uses vascular endothelial cells, which are located in the inner lining of blood vessels. Their extracellular vesicles (EVs), which are small membrane-enclosed components released from the cell, are key to the treatment, but it was unclear exactly how these vesicles function. Harvard University researchers hypothesized that these endothelial extracellular vesicles (EEVs) hold the potential to produce a protective effect on cardiac tissue by acting as messengers to other cells. The researchers mapped all the proteins found in EEVs and discovered specific protein groups that are also present during ischemic preconditioning. They concluded that this similarity signifies these protein groups have an important role in protecting cardiac tissue.
Image Source: qimono
Along with identifying the specific protein groups, researchers observed the EEVs’ effect on IRI through sensors that monitored the contractile functionality, or ability to contract, of myocardial tissue. Contractility of the heart is essential for pumping blood into other organs, and IRI significantly reduces that function. The researchers were able to show that increasing EEV concentrations decreased the number of dead myocardial cells and that the contraction force of cardiac tissues treated with EEVs was four times stronger than without any treatment. Thus, the researchers concluded that EEVs aided in IRI recovery.
This recent study not only provides a deeper understanding of the functions of EEVs, but it also shows the promise of EEVs as a possible therapy that can address the complexities of IRI and reduce the detrimental effects of heart attacks for countless numbers of affected Americans. Through further research on using EEVs in cardiovascular treatment, scientists may find a way to save myocardial cells that would otherwise be forever lost. Moreover, extracellular vesicles show potential in regenerative medicine for other areas such as nervous system disorders, kidney diseases, and cancer therapy, as well as drug delivery. Thus, EVs may be hidden key components to treating other conditions that scientists have not yet found answers for. As research and technology advances, finding out whether EVs do indeed contain even greater capabilities will be a matter of time.
This recent study not only provides a deeper understanding of the functions of EEVs, but it also shows the promise of EEVs as a possible therapy that can address the complexities of IRI and reduce the detrimental effects of heart attacks for countless numbers of affected Americans. Through further research on using EEVs in cardiovascular treatment, scientists may find a way to save myocardial cells that would otherwise be forever lost. Moreover, extracellular vesicles show potential in regenerative medicine for other areas such as nervous system disorders, kidney diseases, and cancer therapy, as well as drug delivery. Thus, EVs may be hidden key components to treating other conditions that scientists have not yet found answers for. As research and technology advances, finding out whether EVs do indeed contain even greater capabilities will be a matter of time.
Featured Image Source: jesse orrico
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|