Gut Enzymes May Help Solve the Blood Shortage Crisis
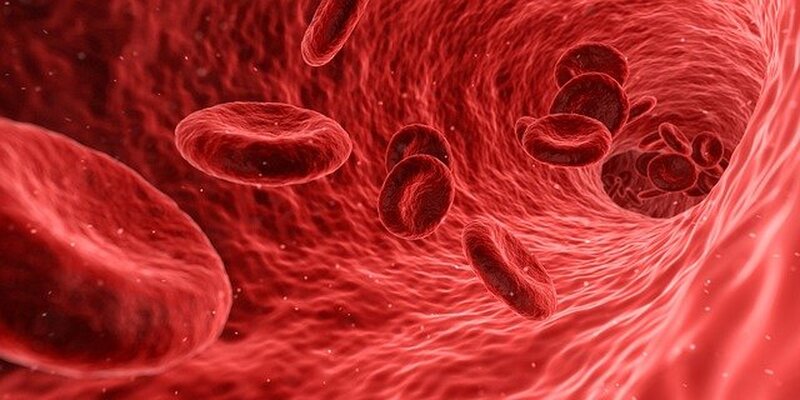
Blood transfusions, the process of introducing the donated blood of one person into the bloodstream of another, are a common and life-saving medical practice first developed during World War 2. The need for blood is widespread, as it is used for treating anything from chronic diseases to acute traumas. The Red Cross currently currently estimates that blood is required by a US patient every 2 seconds, making it critical for hospitals to ensure an adequate supply at all times. Yet despite this need, donated blood cannot immediately be given to every person who might need it. There are four main blood types: A, B, AB, and O. Those with blood type A cannot receive type B blood since the recipient’s cells express surface antigens that recognize the donor’s blood as a foreign intruder, prompting an immediate hemolytic reaction. If this mismatch occurs during a transfusion, it is often lethal for the patient. Blood type O, on the other hand, lacks both A and B antigens, so it remains immunologically invisible and can be safely given to any patient. This makes the O blood type extremely valuable for hospitals, as it can be used in situations where blood is needed quickly but the patient’s blood type is unknown. Still, US hospitals remain with blood shortages, a problem that is further magnified in middle- and low-income countries.
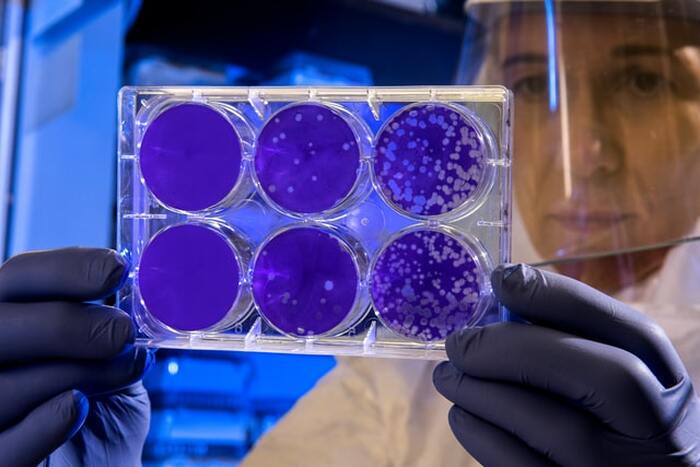
Understanding this problem, researchers at the University of British Columbia sought an efficient enzyme that could remove the type-defining antigen from blood cells. Distinguished by their sugar structures, the UBC researchers reasoned that an enzyme for these antigens would likely be found in microbes inhabiting the sugar-rich digestive system. In their new study, the team collected human stool samples and analyzed the genes of the microbes contained within to determine if they produced enzymes capable of removing these sugars from blood antigens. Using a multi-step analysis, they were able to narrow their search from 800,000 to just eleven possible genes. Each of these were then studied extensively, finding that two enzymes (FpGalNAc deacetylase and FpGalactosaminidase) worked together to change the sugars on blood type A antigens to those that don’t provoke a deadly immune response.
Understanding this problem, researchers at the University of British Columbia sought an efficient enzyme that could remove the type-defining antigen from blood cells. Distinguished by their sugar structures, the UBC researchers reasoned that an enzyme for these antigens would likely be found in microbes inhabiting the sugar-rich digestive system. In their new study, the team collected human stool samples and analyzed the genes of the microbes contained within to determine if they produced enzymes capable of removing these sugars from blood antigens. Using a multi-step analysis, they were able to narrow their search from 800,000 to just eleven possible genes. Each of these were then studied extensively, finding that two enzymes (FpGalNAc deacetylase and FpGalactosaminidase) worked together to change the sugars on blood type A antigens to those that don’t provoke a deadly immune response.
Image Source: CDC
This discovery proved that blood antigens could be changed to artificially increase the supply of O type blood. Furthermore, it also suggested that this process could be done in a direct and cost-effective manner. Other enzymatic methods either resulted in an incomplete conversion or required an impractical amount of enzymes. Moreover, no previously tested enzyme had been shown to function as well in experimental conditions as in actual blood.
Further research is being conducted to ensure both the complete removal of blood antigens and that these blood cells are not functionally compromised. These findings point to an exciting development in medicine, especially in emergency situations where blood transfusion is necessary but the patient's blood type is unknown. Looking beyond the US, this can have significant impacts in low-income countries where the blood donation rate is only 4.4 per 1000 people (compared to 32.6 per 1000 in high-income countries). This research gives hope to millions of people who currently lack access to blood matching their blood type.
Further research is being conducted to ensure both the complete removal of blood antigens and that these blood cells are not functionally compromised. These findings point to an exciting development in medicine, especially in emergency situations where blood transfusion is necessary but the patient's blood type is unknown. Looking beyond the US, this can have significant impacts in low-income countries where the blood donation rate is only 4.4 per 1000 people (compared to 32.6 per 1000 in high-income countries). This research gives hope to millions of people who currently lack access to blood matching their blood type.
Featured Image Source: qimono
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|