COVID-19 Natural Immunity, Reinfection, and Vaccination
As the coronavirus pandemic continues, millions have contracted the disease, and more will continue to do so. Those who have recovered may wonder if they are now immune to the virus and whether they even need the vaccine. In other words, is reinfection with COVID-19 possible in recovered patients, and will the vaccine provide protection against such reinfection?
Researchers in South Korea attempted to answer the first of these questions about COVID-19 reinfection using six patients who retested positive for COVID-19 following recovery. The tests were conducted through nose and mouth swabs during the first diagnosis of COVID and after recovery. The swabs collect samples from the upper respiratory tract; however, COVID-19 uses a protein to enter cells (called angiotensin-converting enzyme 2 or ACE2) that is more abundant in the lower respiratory tract. Thus, later positive retests following negative results may occur if any remaining virus is transferred to the nose and mouth from the lungs when patients cough. This could have been the case in six out of the seven positive retests in the study, which the researchers, following genome sequencing, concluded to be due to remaining dead virus fragments.
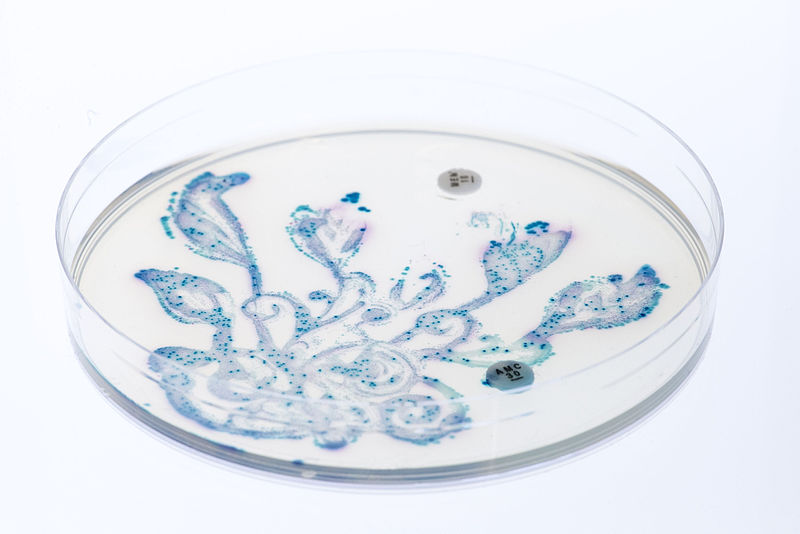
In one patient, however, genome mapping of the second infection sample revealed a different variant of COVID-19 from the initial diagnosis. The rise and fall of the patient’s antibodies during the potential reinfection also matched the general trend seen in patients with mild COVID-19 infection. Furthermore, the strain variant noted in the two COVID infections matched the emergence timepoints of the strains: the initial infection on March 5, 2020 was due to a strain common in South Korea from late February to early March 2020, while the latter infection observed on April 5, 2020 occurred due to a strain that appeared in early April 2020. These findings suggest that the positive retest in this patient was due to reinfection with COVID-19.
Researchers in South Korea attempted to answer the first of these questions about COVID-19 reinfection using six patients who retested positive for COVID-19 following recovery. The tests were conducted through nose and mouth swabs during the first diagnosis of COVID and after recovery. The swabs collect samples from the upper respiratory tract; however, COVID-19 uses a protein to enter cells (called angiotensin-converting enzyme 2 or ACE2) that is more abundant in the lower respiratory tract. Thus, later positive retests following negative results may occur if any remaining virus is transferred to the nose and mouth from the lungs when patients cough. This could have been the case in six out of the seven positive retests in the study, which the researchers, following genome sequencing, concluded to be due to remaining dead virus fragments.
In one patient, however, genome mapping of the second infection sample revealed a different variant of COVID-19 from the initial diagnosis. The rise and fall of the patient’s antibodies during the potential reinfection also matched the general trend seen in patients with mild COVID-19 infection. Furthermore, the strain variant noted in the two COVID infections matched the emergence timepoints of the strains: the initial infection on March 5, 2020 was due to a strain common in South Korea from late February to early March 2020, while the latter infection observed on April 5, 2020 occurred due to a strain that appeared in early April 2020. These findings suggest that the positive retest in this patient was due to reinfection with COVID-19.
Image Source: geralt
The findings of this study thus imply that COVID-19 infection may not give patients immunity to a different strain of the virus. It must be noted, however, that due to the small sample size of this study, the conclusions may need additional investigation. A review of various studies regarding COVID-19 reinfection suggests that positive test results may be due to a number of factors including the method of testing, underlying diseases, and viral transfer from the lower respiratory tract to the upper respiratory tract due to coughing. However, one study mentioned in the review also estimated that immunity following infection with COVID-19 lasts only about 40 days, and findings from previous coronavirus studies imply that different strains of coronavirus can cause reinfection following recovery.
These findings suggest it is likely worthwhile for even recovered patients to receive the COVID-19 vaccine. A study using ferrets found that a COVID-19 vaccine candidate was not any less effective against a mutated strain of virus (D614G mutation) than strains without the mutation. While it is also unclear how long immunity from the vaccine will last, National Public Radio reports that COVID-19 immunity can last for many months; other sources suggest that there could be 2–3 years of immunity conferred through an annual shot. The bottom line: for longer-lasting and more broad immunity to COVID-19 strains, a vaccine is probably beneficial even for recovered patients.
These findings suggest it is likely worthwhile for even recovered patients to receive the COVID-19 vaccine. A study using ferrets found that a COVID-19 vaccine candidate was not any less effective against a mutated strain of virus (D614G mutation) than strains without the mutation. While it is also unclear how long immunity from the vaccine will last, National Public Radio reports that COVID-19 immunity can last for many months; other sources suggest that there could be 2–3 years of immunity conferred through an annual shot. The bottom line: for longer-lasting and more broad immunity to COVID-19 strains, a vaccine is probably beneficial even for recovered patients.
Image Source: torstensimon
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|