CDC Guidelines for Pediatric Mild Traumatic Brain Injury Treatment
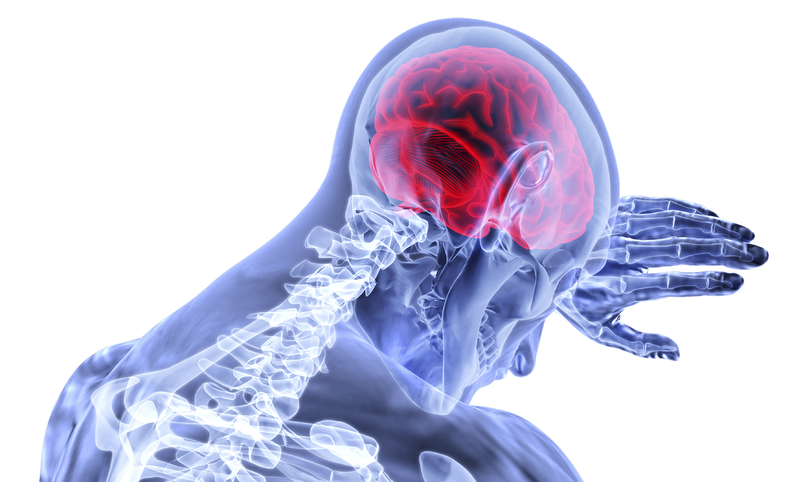
Infants and children between the ages of 1 and 4 visit the ED for traumatic brain injury (TBI) at twice the rate of adults. Any loss of consciousness, confusion, or disorientation lasting under 30 minutes is classified as mild traumatic brain injury (mTBI), which often occurs after a blow to the head. There has been an increase in mTBI cases by about 140% from 2007 to 2013 for children ages 14 and under.
With the apparent rise in number of pediatric mTBI, this specific type of injury has been receiving news coverage recently due to its frequency in sports, such as football, and its lasting impact in case of multiple mTBIs. For parents, it is important to know that they are also a common problem in children and hence a matter to be taken seriously. Children can suffer mTBIs from playing on the playground or participating in sports.
Pediatric mTBI is most often associated with concussions. Concussions vary in severity, but if the symptoms are short-term and not threatening, it is classified as mild. Symptoms include headaches, vision problems, memory loss, dizziness, and more. Often, children may not realize that something is wrong or may be unable to express the severity of the condition. Recognizing symptoms in children suffering from mTBI is essential to getting proper and timely treatment. It is also crucial to understand risk factors and prevention methods, especially if a child is involved in a contact sport.
Pediatric mTBI usually has short term effects lasting up to three months. However, there are potential long term effects that can negatively influence a child’s ability to function properly for up to three years. In such cases, children may experience changes in their thought process, sensation, communicating abilities, and emotions. mTBI is also considered a risk factor for developing dementia.
With the apparent rise in number of pediatric mTBI, this specific type of injury has been receiving news coverage recently due to its frequency in sports, such as football, and its lasting impact in case of multiple mTBIs. For parents, it is important to know that they are also a common problem in children and hence a matter to be taken seriously. Children can suffer mTBIs from playing on the playground or participating in sports.
Pediatric mTBI is most often associated with concussions. Concussions vary in severity, but if the symptoms are short-term and not threatening, it is classified as mild. Symptoms include headaches, vision problems, memory loss, dizziness, and more. Often, children may not realize that something is wrong or may be unable to express the severity of the condition. Recognizing symptoms in children suffering from mTBI is essential to getting proper and timely treatment. It is also crucial to understand risk factors and prevention methods, especially if a child is involved in a contact sport.
Pediatric mTBI usually has short term effects lasting up to three months. However, there are potential long term effects that can negatively influence a child’s ability to function properly for up to three years. In such cases, children may experience changes in their thought process, sensation, communicating abilities, and emotions. mTBI is also considered a risk factor for developing dementia.
Image Source: valelopardo
Treatment of pediatric mTBI is often inconsistent due to lack of standardization and evidence-based approaches. Some doctors choose to treat symptoms, while others take a more direct approach. Diagnosis procedures have also differed due to disagreements about the necessity of neuroimaging. This leads to variations in treatment and recovery process, with the underlying problem being an insufficient understanding of the impacts of mTBIs. Since each case presents different symptoms and severity, doctors must adjust their practice accordingly.
Recently, the Centers for Disease Control and Prevention (CDC) compiled over 25 years’ worth of set guidelines for diagnosis and treatment of pediatric mTBI. The guideline references 34,000 articles in an attempt to optimize the approach to treating pediatric mTBI. It instructs clinicians—specifically those in the emergency department—on the diagnosis, prognosis, management, and treatment of mTBI.
Pediatric mTBI treatment is focused on controlling symptoms. By setting a standard for the care of mTBI, the CDC hopes to eliminate differentiating patterns of treatment. Physicians are recommended to not only rely on routine imaging for diagnosis, but to also consider the risk factors outlined in the guideline. To assist with improving care and treatment of mTBI, the CDC also created resources for parents, such as pamphlets and brochures that contain information about what to expect when children are diagnosed with mTBI, when to request CT imaging, and what parents can do to help with recovery. These resources allow parents to be informed about the condition and recognize signs of escalating severity. They also highlight the importance of proper diagnosis followed by the parents’ understanding of the recovery process. As more recent research finds that mTBIs have long term impacts on a child’s neural development and cognitive abilities, the CDC guidelines will assist in shaping a reliable standard of care for pediatric patients with mTBI.
Recently, the Centers for Disease Control and Prevention (CDC) compiled over 25 years’ worth of set guidelines for diagnosis and treatment of pediatric mTBI. The guideline references 34,000 articles in an attempt to optimize the approach to treating pediatric mTBI. It instructs clinicians—specifically those in the emergency department—on the diagnosis, prognosis, management, and treatment of mTBI.
Pediatric mTBI treatment is focused on controlling symptoms. By setting a standard for the care of mTBI, the CDC hopes to eliminate differentiating patterns of treatment. Physicians are recommended to not only rely on routine imaging for diagnosis, but to also consider the risk factors outlined in the guideline. To assist with improving care and treatment of mTBI, the CDC also created resources for parents, such as pamphlets and brochures that contain information about what to expect when children are diagnosed with mTBI, when to request CT imaging, and what parents can do to help with recovery. These resources allow parents to be informed about the condition and recognize signs of escalating severity. They also highlight the importance of proper diagnosis followed by the parents’ understanding of the recovery process. As more recent research finds that mTBIs have long term impacts on a child’s neural development and cognitive abilities, the CDC guidelines will assist in shaping a reliable standard of care for pediatric patients with mTBI.
Featured Image Source: VSRao
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|