Allergies in Dogs and their Owners
From rural to urban settings, the types of daily interactions people have with domesticated animals, plants, and wildlife differ in many ways. These interactions can have measurable impacts on the health of people in these communities. Animal models, such as mice or rats, can help researchers follow the progression of a human disease in a laboratory setting. While a disease can be recreated relatively well in an animal model, it is more difficult to replicate the diverse environmental factors that shape the health of humans and their communities. The Centers for Disease Control and Prevention has adopted the One Health approach, which recognizes the interconnection between animals, humans, and their shared environment. Changes in climate and where people live have resulted in conditions where zoonotic diseases, or diseases spread between animals and people, are more likely to occur. The environment humans and their pets share can also have similar effects on their health. Non-communicable diseases (noninfectious diseases like diabetes) and long-term stressors can occur simultaneously in people and their pets. Because of this, researchers are interested in the potential of pet dogs as models of diseases related to environmental exposures.
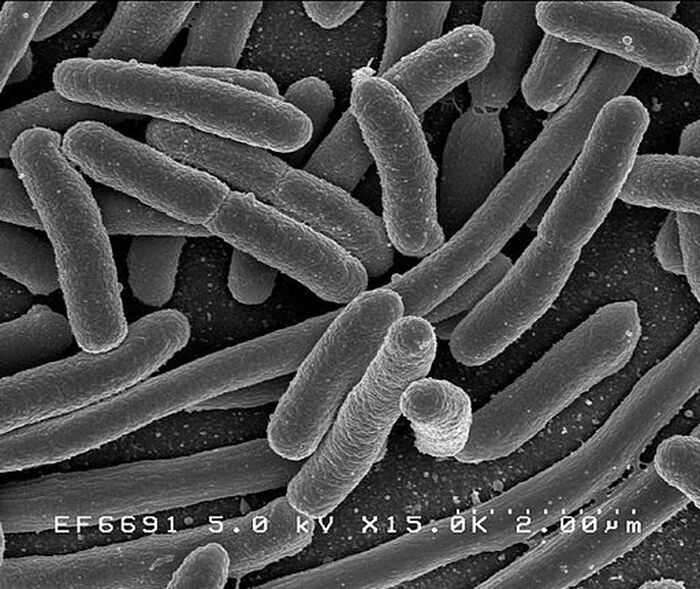
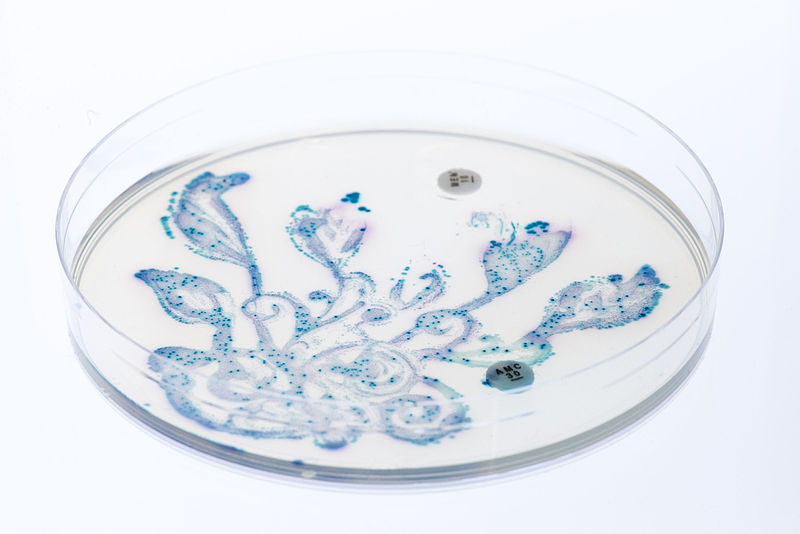
One non-communicable disease of interest due to its direct connection to the environment is allergic rhinitis (hay fever), among other allergic disorders. Finnish scientists collected samples from 168 dog-owner pairs, some with allergies and some without, in order to analyze shared allergic traits and how allergies were associated with their living environments. The dog-owner pairs lived in a variety of locations, from urban to rural, where lifestyle and environment were documented as two separate factors to account for nuanced environmental exposures. The researchers took skin, fecal, and whole blood samples from the dogs and their owners in order to compare the skin and gut microbiotas of dogs and humans living in different areas. Microorganisms on the skin and in the gut reflect the external environment of their host organism, and an overabundance or deficiency of certain types of bacteria are associated with some diseases and conditions. The human participants also answered a survey about their own possible allergy symptoms as well as the possible allergy symptoms of their dogs.
One non-communicable disease of interest due to its direct connection to the environment is allergic rhinitis (hay fever), among other allergic disorders. Finnish scientists collected samples from 168 dog-owner pairs, some with allergies and some without, in order to analyze shared allergic traits and how allergies were associated with their living environments. The dog-owner pairs lived in a variety of locations, from urban to rural, where lifestyle and environment were documented as two separate factors to account for nuanced environmental exposures. The researchers took skin, fecal, and whole blood samples from the dogs and their owners in order to compare the skin and gut microbiotas of dogs and humans living in different areas. Microorganisms on the skin and in the gut reflect the external environment of their host organism, and an overabundance or deficiency of certain types of bacteria are associated with some diseases and conditions. The human participants also answered a survey about their own possible allergy symptoms as well as the possible allergy symptoms of their dogs.
The researchers found that when allergies were present, they frequently occurred in both the dog and the owner within the pair (and likewise, an owner without allergic traits often had a dog that also had no allergic traits.) This was consistent with prior research. Based on the results of the survey, dog owners in urban areas reported higher allergic symptoms in themselves and their dogs than dog owners in rural areas. When humans have less exposure to animals and their microbiotas, it is thought to contribute to an increased frequency in allergies. The skin microbiota in both humans and dogs was more greatly impacted by the environment than the gut microbiota. Despite these findings, the researchers did not find a significant microbial signal that was associated with allergies in humans and their dogs. Additionally, many complex factors, like air pollution, could not be taken into account with measurements of microorganisms alone.
The higher amount of allergy symptoms reported in the dog owners living in urban areas and the co-occurrence of allergy symptoms in dogs and their owners point to shared environmental exposures. Future studies assessing the microbiomes of humans and animals may illuminate connections between bacteria, diet, environment, and disease that could change the way people live and interact with the world around them. Recognition of the connectedness between humans, animals, and the environment will lead to more research that enhances understanding of noncommunicable diseases and how to promote healthy communities.
The higher amount of allergy symptoms reported in the dog owners living in urban areas and the co-occurrence of allergy symptoms in dogs and their owners point to shared environmental exposures. Future studies assessing the microbiomes of humans and animals may illuminate connections between bacteria, diet, environment, and disease that could change the way people live and interact with the world around them. Recognition of the connectedness between humans, animals, and the environment will lead to more research that enhances understanding of noncommunicable diseases and how to promote healthy communities.
Featured Image Source: Lepale
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|