Allergic to Exercise: The Reality of Exercise-Induced Anaphylaxis
Exercise-induced anaphylaxis (EIA) is a rare disorder in which anaphylaxis is triggered due to exercise. Anaphylaxis is a severe, potentially fatal, allergic reaction caused by a particular allergen. Common allergens include peanuts, wheat, shellfish, and many more. Anaphylaxis is usually treated by administering epinephrine through an epipen. About 5-15% of anaphylactic cases are due to EIA.
While a particular activity or intensity level has not been identified for the onset of anaphylaxis, it is most often caused by moderately intensive jogging. Other activities that have been correlated with EIA are aerobics, walking, and tennis. No genetic link has been identified for EIA; the cases are most often sporadic. Interestingly, studies have found that the ratio of females to males with EIA is two to one.
Food-dependent exercise-induced anaphylaxis (FDEIA) is a subset of EIA; around one- third to one-half of EIA cases are food-based. Patients with FDEIA will develop symptoms of anaphylaxis only if they exercise within minutes to hours of ingesting certain food. It has also been observed that FDEIA can occur when that specific food is consumed after exercising: this lead scientists to believe that development of FDEIA is due more to the interaction between the food and exercise rather than the sequence of events.
While a particular activity or intensity level has not been identified for the onset of anaphylaxis, it is most often caused by moderately intensive jogging. Other activities that have been correlated with EIA are aerobics, walking, and tennis. No genetic link has been identified for EIA; the cases are most often sporadic. Interestingly, studies have found that the ratio of females to males with EIA is two to one.
Food-dependent exercise-induced anaphylaxis (FDEIA) is a subset of EIA; around one- third to one-half of EIA cases are food-based. Patients with FDEIA will develop symptoms of anaphylaxis only if they exercise within minutes to hours of ingesting certain food. It has also been observed that FDEIA can occur when that specific food is consumed after exercising: this lead scientists to believe that development of FDEIA is due more to the interaction between the food and exercise rather than the sequence of events.
Image Source: Joe Raedle
The symptoms of EIA and FDEIA are similar to those of anaphylaxis: itching, hives, flushing, and shortness of breath. If the exercise is continued, gastrointestinal symptoms such as cramps, vomiting, nausea, and a feeling of choking can emerge. The severity of symptoms increases for fully developed EIA and can result in cardiovascular symptoms, such as the loss of consciousness. Though EIA is bth rarely fatal and near fatal, it is still a life-threatening condition. EIA symptoms are most often noticed in patients during early adulthood; however, EIA is found in patients anywhere between five to 75 years.
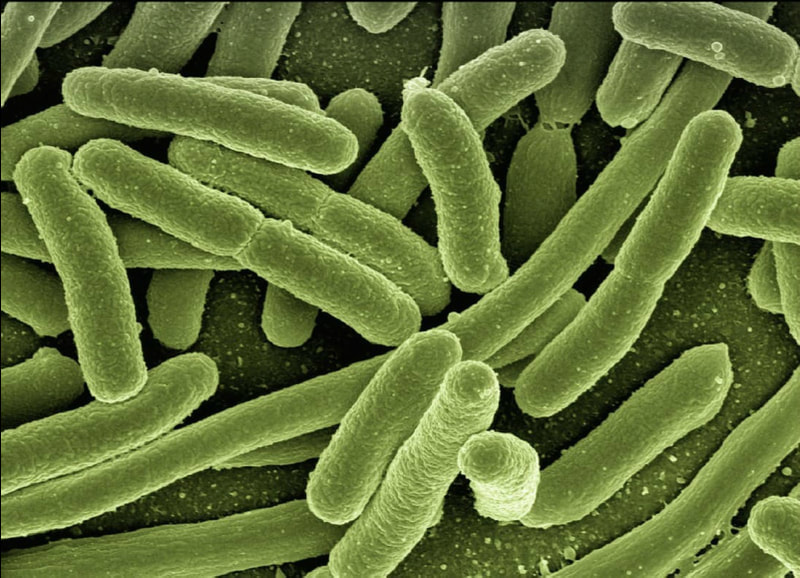
Scientists are not certain of the pathophysiology of EIA and FDEIA. However, they are certain, as with all cases of anaphylaxis, that a prominent feature is histamine release by mast cells. Because of the lack of understanding behind the mechanics of EIA, there is no known cure for this disorder. However, stopping the activity early usually leads to improvement. Continuing the physical activity after experiencing symptoms of EIA will exacerbate symptoms and require pharmacotherapy, such as epinephrine, antihistamines, and systemic corticosteroids. It is important to seek medical attention from a healthcare provider after the onset of EIA.
Though there is no treatment, there are numerous methods to help prevent EIA from developing. Patients should generally avoid physical activity during extreme weather or during allergy season when the pollen count is high. It is also important not to take aspirin or other nonsteroidal anti-inflammatory drugs in conjunction with exercise. For patients with FDEIA in particular, it is advised not to exercise four to six hours after eating and not to eat directly after completing physical activity. In some cases, pharmacological protection is effective. Since anaphylaxis causes mast cell degranulation, taking pharmaceuticals that inhibit cell degranulation could prevent the onset of FDEIA.
As new technologies are invented and more research is devoted to understanding the biology behind EIA and FDEIA, a cure can hopefully be discovered.
Scientists are not certain of the pathophysiology of EIA and FDEIA. However, they are certain, as with all cases of anaphylaxis, that a prominent feature is histamine release by mast cells. Because of the lack of understanding behind the mechanics of EIA, there is no known cure for this disorder. However, stopping the activity early usually leads to improvement. Continuing the physical activity after experiencing symptoms of EIA will exacerbate symptoms and require pharmacotherapy, such as epinephrine, antihistamines, and systemic corticosteroids. It is important to seek medical attention from a healthcare provider after the onset of EIA.
Though there is no treatment, there are numerous methods to help prevent EIA from developing. Patients should generally avoid physical activity during extreme weather or during allergy season when the pollen count is high. It is also important not to take aspirin or other nonsteroidal anti-inflammatory drugs in conjunction with exercise. For patients with FDEIA in particular, it is advised not to exercise four to six hours after eating and not to eat directly after completing physical activity. In some cases, pharmacological protection is effective. Since anaphylaxis causes mast cell degranulation, taking pharmaceuticals that inhibit cell degranulation could prevent the onset of FDEIA.
As new technologies are invented and more research is devoted to understanding the biology behind EIA and FDEIA, a cure can hopefully be discovered.
Featured Image Source: Pixabay
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|