A Tale of Two Viruses: Comparing COVID-19 to the Swine Flu
People everywhere are currently living through a global pandemic of COVID-19, a respiratory disease caused by the novel SARS-CoV-2 virus. The virus, which originated in China and has since spread throughout the world, has infected 1.67 million and killed over 124,000 individuals in the United States alone (as of June 23, 2020). As societies try to understand the strict regulations imposed by the U.S government, including orders to stay inside and practice social distancing, many have begun looking at the last major pandemic for answers: the H1N1 “Swine Flu” influenza pandemic of 2009.
Both the H1N1 influenza and COVID-19 infections affect the respiratory tract and can lead to pneumonia, fever, cough, headaches, chills, body aches, and sometimes vomiting and diarrhea. The H1N1 influenza notoriously infected 60.8 million individuals and killed 12,469 people in the United States. This viral outbreak, however, was unique in that it primarily affected younger individuals—most people over the age of 60 had developed immunity from prior exposures to older H1N1 strains across their lifetime. The U.S government also responded swiftly to the development of the H1N1 influenza. Within one week of the first reported H1N1 case in the United States, the Centers for Disease Control and Prevention (CDC) declared a public health emergency. By the end of the month, the H1N1 influenza was declared a national pandemic. The CDC was also able to quickly develop accurate testing kits that could be shared internationally.
Both the H1N1 influenza and COVID-19 infections affect the respiratory tract and can lead to pneumonia, fever, cough, headaches, chills, body aches, and sometimes vomiting and diarrhea. The H1N1 influenza notoriously infected 60.8 million individuals and killed 12,469 people in the United States. This viral outbreak, however, was unique in that it primarily affected younger individuals—most people over the age of 60 had developed immunity from prior exposures to older H1N1 strains across their lifetime. The U.S government also responded swiftly to the development of the H1N1 influenza. Within one week of the first reported H1N1 case in the United States, the Centers for Disease Control and Prevention (CDC) declared a public health emergency. By the end of the month, the H1N1 influenza was declared a national pandemic. The CDC was also able to quickly develop accurate testing kits that could be shared internationally.
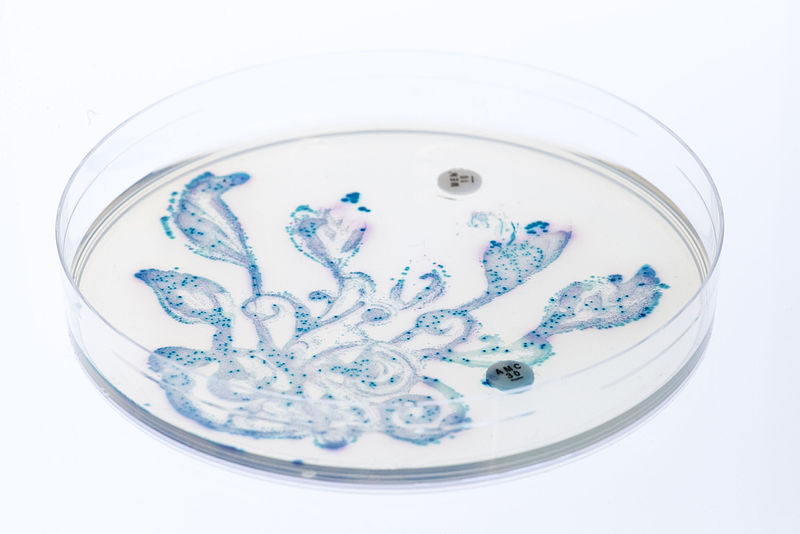
Image Source: Melissa Jeanty
Unlike influenza, nobody is able to benefit from a preexisting immunity against COVID-19, as this is a novel virus that has not previously infected others. As a result, it is a highly contagious viral pneumonia that endangers all who contract it. Of primary concern is its effect on individuals who are elderly, immunocompromised, or have specific underlying medical conditions such as diabetes, heart disease, and lung disease. The CDC is currently recommending that people frequently wash their hands, avoid touching their face, and social distance to fight COVID-19. This is particularly important as SARS-CoV-2 has more recently been shown to be an airborne virus that may live on surfaces for up to seven days. However, people did not see the same strict enforcement of recommendations and orders set in place during the 2009 influenza.
With the coronavirus, however, testing is limited and many who wish to be tested are unable to. In the United States, the coronavirus has an indicated fatality rate of at least 0.8% while the H1N1 influenza had a mortality rate of 0.02%. COVID-19 also appears to spread more easily than H1N1 and carriers of the disease may remain asymptomatic, continuing to unknowingly spread the disease without any symptoms. New research is currently being done to find a vaccine against the virus, a vital need as COVID-19 has a dramatically higher mortality rate among older individuals and those with pre-existing health conditions. Ultimately, the United States’ quicker response to the H1N1 virus and the preexisting immunity in many older individuals resulted in a lower death rate. We can do our part to minimize the impact of COVID-19 by staying home, practicing social distancing, wearing masks, and washing our hands.
With the coronavirus, however, testing is limited and many who wish to be tested are unable to. In the United States, the coronavirus has an indicated fatality rate of at least 0.8% while the H1N1 influenza had a mortality rate of 0.02%. COVID-19 also appears to spread more easily than H1N1 and carriers of the disease may remain asymptomatic, continuing to unknowingly spread the disease without any symptoms. New research is currently being done to find a vaccine against the virus, a vital need as COVID-19 has a dramatically higher mortality rate among older individuals and those with pre-existing health conditions. Ultimately, the United States’ quicker response to the H1N1 virus and the preexisting immunity in many older individuals resulted in a lower death rate. We can do our part to minimize the impact of COVID-19 by staying home, practicing social distancing, wearing masks, and washing our hands.
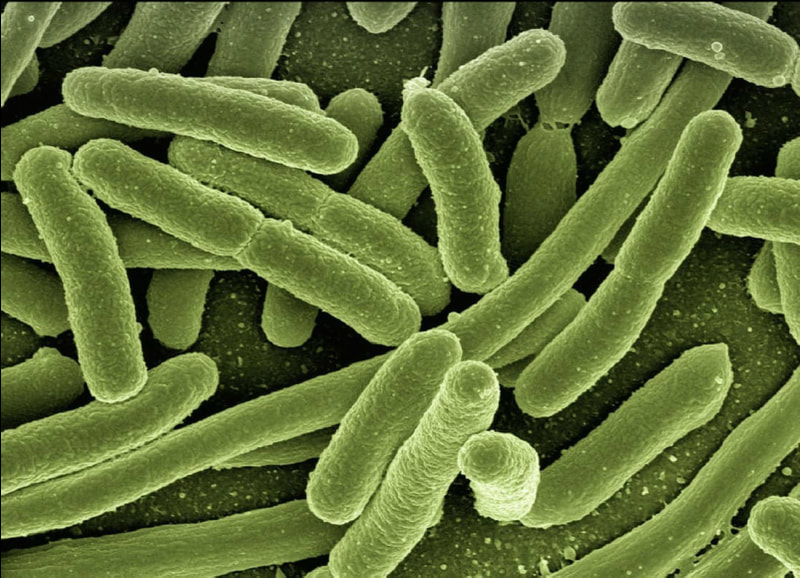
Featured Image Source: enriquelopezgarre
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|