A Possibly Unnecessary Aspect of Gynecologist Appointments: Cervical Cancer
Every year, millions of women in the United States visit their doctors for one test: the annual pelvic examination. Specifically, these annual pelvic examinations involve two main tests to screen for cervical cancer. For the first test, the bimanual pelvic examination, a trained physician applies pressure on the abdomen and pelvic region to check if the internal pelvic organs are functioning properly. For the second test, called the Pap test, a metal tool collects cells from the cervix to screen for cervical cancer. These tests undoubtedly require time and cost about $40 per exam, but are still widely considered a necessary aspect of sex health.
While these medical tests are indeed important, many medical organizations, such as the American College of Obstetricians and Gynecologists and the American Cancer Society, do not recommend these screenings for women who are younger than 21 years old. Since cervical cancer usually affects women older than the age of 35, women under the age of 21 would not likely need these tests. Testing would be required if the patient was exhibiting symptoms of cervical cancer, such as light bleeding between periods or unexplained pelvic pain.
Despite this advice from the American College of Obstetricians and Gynecologists and the American Cancer Society, it is still unclear whether young women are visiting their physicians for possibly unnecessary pelvic examinations. In one study conducted by the Center of Disease Control and Prevention (CDC), researchers investigated the rates at which female patients visited their local doctors for these tests in 2020 to determine whether these tests were truly indicative of cervical cancer.
While these medical tests are indeed important, many medical organizations, such as the American College of Obstetricians and Gynecologists and the American Cancer Society, do not recommend these screenings for women who are younger than 21 years old. Since cervical cancer usually affects women older than the age of 35, women under the age of 21 would not likely need these tests. Testing would be required if the patient was exhibiting symptoms of cervical cancer, such as light bleeding between periods or unexplained pelvic pain.
Despite this advice from the American College of Obstetricians and Gynecologists and the American Cancer Society, it is still unclear whether young women are visiting their physicians for possibly unnecessary pelvic examinations. In one study conducted by the Center of Disease Control and Prevention (CDC), researchers investigated the rates at which female patients visited their local doctors for these tests in 2020 to determine whether these tests were truly indicative of cervical cancer.
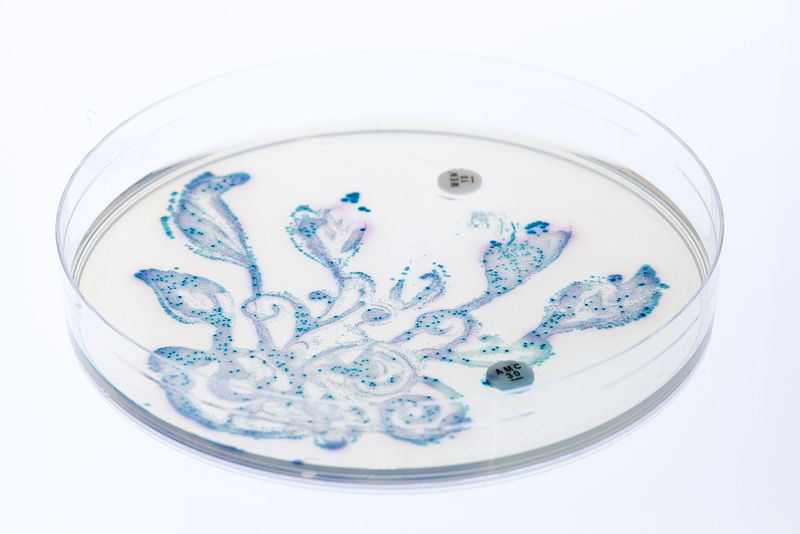
Image Source: Priscilla Du Perez
In the study, the CDC analyzed surveys of 3040 adolescent girls and young women between the ages of 15 and 20 years in the United States. In these surveys, the female respondents were asked whether they received a bimanual pelvic examination by a doctor or nurse, which involve a medical professional inserting their hand inside the vagina of the patient to apply pressure on their organs. Another question asked whether the respondent had a medical instrument inserted inside their vagina, or a Pap test. Finally, the respondents were asked whether these tests were conducted within the last year and the reason for these tests.
Based on the respondents’ answers, the researchers organized four reasons that would make a Pap test or bimanual pelvic examination necessary given the cancer societies’ recommendations: pregnancy, IUD use, a medical problem, or treatment of a sexually transmitted infection. If a respondent did not list any of these reasons for their pelvic examination, the researchers deemed their examination as unnecessary.
From the survey’s results, 22.9% of the respondents reported receiving a bimanual pelvic examination within the last year. Furthermore, 34.9% of these reports were deemed potentially unneeded. Additionally, 19.2% of the survey respondents reported receiving a Pap test within the last year, and 71.9% of these respondents’ tests were deemed potentially unnecessary. Interestingly, 97.7% of the reported nonessential bimanual pelvic examinations were conducted in the same doctor’s visit as the nonessential Pap test, meaning that many of these exorbitant tests are ordered at the same time without further consideration by patients and health officials about whether they are truly needed,
From these findings, the study reiterates that despite physician recommendations, potentially unnecessary pelvic examinations are still being conducted. While it may seem that these tests are “better safe than sorry,” each screening pelvic examination averages to $40 per examination with healthcare. In total, the United States alone spends $123 million on potentially pelvic screenings per year. Notably, for young women who do not express symptoms of cervical cancer, these unneeded tests are not only costly monetarily, but an inefficient use of time and resources.
Based on the CDC’s findings, exorbitant pelvic examinations are conducted every year, costing taxpayer dollars and patient time. While women are still recommended to be screened for cervical cancer past the age of 21, younger women who do not experience symptoms may not need to undergo these possibly invasive and uncomfortable examinations every year.
Based on the respondents’ answers, the researchers organized four reasons that would make a Pap test or bimanual pelvic examination necessary given the cancer societies’ recommendations: pregnancy, IUD use, a medical problem, or treatment of a sexually transmitted infection. If a respondent did not list any of these reasons for their pelvic examination, the researchers deemed their examination as unnecessary.
From the survey’s results, 22.9% of the respondents reported receiving a bimanual pelvic examination within the last year. Furthermore, 34.9% of these reports were deemed potentially unneeded. Additionally, 19.2% of the survey respondents reported receiving a Pap test within the last year, and 71.9% of these respondents’ tests were deemed potentially unnecessary. Interestingly, 97.7% of the reported nonessential bimanual pelvic examinations were conducted in the same doctor’s visit as the nonessential Pap test, meaning that many of these exorbitant tests are ordered at the same time without further consideration by patients and health officials about whether they are truly needed,
From these findings, the study reiterates that despite physician recommendations, potentially unnecessary pelvic examinations are still being conducted. While it may seem that these tests are “better safe than sorry,” each screening pelvic examination averages to $40 per examination with healthcare. In total, the United States alone spends $123 million on potentially pelvic screenings per year. Notably, for young women who do not express symptoms of cervical cancer, these unneeded tests are not only costly monetarily, but an inefficient use of time and resources.
Based on the CDC’s findings, exorbitant pelvic examinations are conducted every year, costing taxpayer dollars and patient time. While women are still recommended to be screened for cervical cancer past the age of 21, younger women who do not experience symptoms may not need to undergo these possibly invasive and uncomfortable examinations every year.
Featured Image Source: Priscilla Du Perez
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|