A New Predictive Model for Detecting Metastatic Cancer
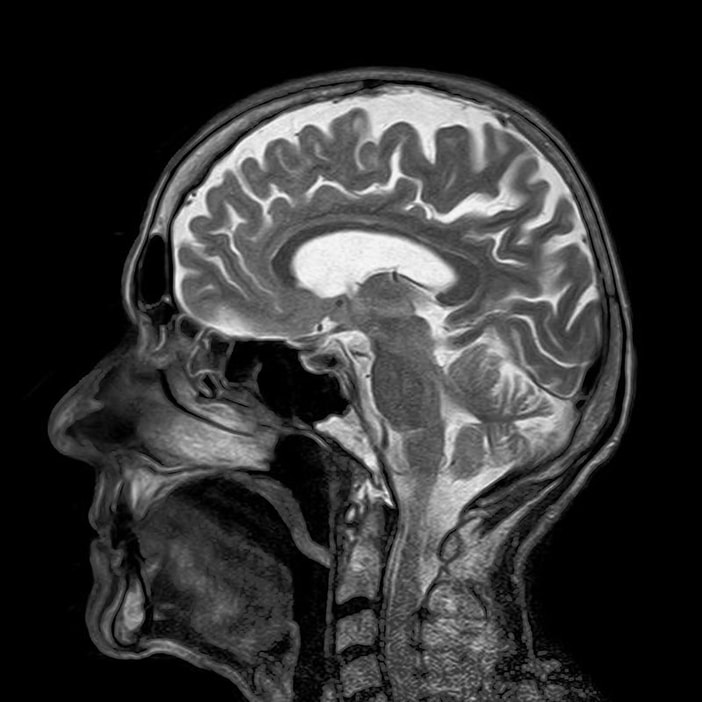
Endometrial cancer is among the most common of gynecological cancers in industrialized countries, with incidence rates steadily rising throughout recent years. Due to its noninvasive and painless nature, doctors rely on magnetic resonance imaging (MRI) as one of the standard diagnostic tools for visualizing cancerous conditions in patients. One important area of examination are the lymph nodes, where the metastasis of cancer cells may indicate a more aggressive tumor. However, lymph node metastasis (LNM) rates are low in early stage endometrial cancer, and unnecessary surgery to remove the lymph nodes may lead to additional complications. Additionally, MRI only provides a 25–50% sensitivity in detecting LNM. To counteract these problems, researchers in China have developed a predictive model that combines MRI scans and clinical parameters to help doctors forecast the presence of LNM in normal-sized lymph nodes.
Image Source: toubibe
The researchers first looked to radiomics, which uses algorithms to extract quantitative features such as shape and density from images. Their study then gathered data on 200 endometrial cancer patients who had been treated between 2011 and 2017. They further divided 140 patients into a training group and 60 patients into a test group. After radiologists manually segmented the tumor regions from MRI slices and created 3D reconstructions, the researchers were able to employ their algorithms to select the desired features. They developed four separate models that utilized different combinations of radiomic features and clinical parameters. These models were evaluated based on their receiver operating characteristic (ROC) curves, which graphically represent a model’s probability of correctly forecasting a true outcome.
One model in particular demonstrated significant predictive ability in analyzing normal-sized lymph nodes for metastasis, outperforming both the other models as well as reports made by radiologists. This model was found to have a 7.8% better accuracy and a 175.3% better sensitivity than radiologists themselves. Other models were found to have slightly higher sensitivities but lower accuracy.
While their data looks promising, the researchers note several limitations in their study. First is the difficulty in obtaining stable radiomic features across samples due to differences in MRI scanner settings and models across the world. Without similar imaging quality, their current models are not reliable. Additionally, the researchers conducted their study without any external validation, meaning that they are unable to confidently apply their findings to patients outside this individual study. Finally, their models do not take into account the genetic information of the patients, which could pose different interpretations of the overall disease outlook.
Regardless, this study brings us one step closer to a future where doctors have access to programs that can detect what the human eye cannot. While it is difficult to determine when such models will become a dependable part of modern medicine, researchers continue to develop new and improved techniques for disease modeling.
One model in particular demonstrated significant predictive ability in analyzing normal-sized lymph nodes for metastasis, outperforming both the other models as well as reports made by radiologists. This model was found to have a 7.8% better accuracy and a 175.3% better sensitivity than radiologists themselves. Other models were found to have slightly higher sensitivities but lower accuracy.
While their data looks promising, the researchers note several limitations in their study. First is the difficulty in obtaining stable radiomic features across samples due to differences in MRI scanner settings and models across the world. Without similar imaging quality, their current models are not reliable. Additionally, the researchers conducted their study without any external validation, meaning that they are unable to confidently apply their findings to patients outside this individual study. Finally, their models do not take into account the genetic information of the patients, which could pose different interpretations of the overall disease outlook.
Regardless, this study brings us one step closer to a future where doctors have access to programs that can detect what the human eye cannot. While it is difficult to determine when such models will become a dependable part of modern medicine, researchers continue to develop new and improved techniques for disease modeling.
Featured Image Source: Markus Spiske
RELATED ARTICLES
|
Vertical Divider
|
Vertical Divider
|
Vertical Divider
|